



| By Dr. Ronald Hoffman

Last week we were assailed with yet another pop science diet report:
“Healthy foods more important than type of diet to reduce heart disease risk: Researchers compare three popular diets and find all three reduce heart disease” reports Science Daily.
So why are you even reading this article? Give up trying to figure out nutrition and leave it to the professionals at Harvard where this study was performed. The implication is that it doesn’t really matter what you eat, as long as it’s reasonably wholesome and not outright highly-processed junk.
Don’t worry about carbs or fat; just eat a “balanced” diet (whatever that is). Or, to echo Michael Pollan’s famous meme from his book Omnivores’ Dilemma: “Eat food. Not too much. Mostly plants.”
Forget about the heated Twitter wars pitting militant vegans vs. dyed-in-the-wool carnivores; Low-fat acolytes vs. Keto stalwarts; Ornish followers vs. Atkins fans.
Stop agonizing over macronutrient ratios, they say. Just shmear some low-fat cream cheese on that whole-grain bagel—according to eminent Harvard researchers, you’re deluding yourself if you think you can avert America’s leading cause of death by obsessively juggling carbs, fats, and proteins.
REALLY??
The so-called OmniHeart trial supports a sort of wimpy dietary nihilism based on a very flawed research design.
Its conclusions are based on a very small cohort (~150 participants) studied over a very short time (2 years).
They didn’t even look at actual cardiac outcomes, but rather at certain blood test values like low density lipoprotein (LDL) cholesterol, C-reactive protein, and cardiac troponin that are thought to be predictive of cardiac risk.
They didn’t evaluate whether patients suffered actual heart problems, required stents or bypasses, or died of heart disease.
They placed the test subjects on three different diets, and then compared blood test results. The claim is that the experimental diets were representative of low-fat vs. low-carb diets currently invoked for cardiovascular prevention.
But that assertion is laughable. Their base diet was the ultra low-fat and low-protein DASH diet often recommended for hypertension. It consists of plentiful whole grains, fruits, vegetables, low-fat dairy, fish and skinless white meat poultry. There’s virtually no fat or sodium. It’s kind of like the Pritikin Diet. Over half of its calories come from carbs.
To this base diet they swapped calories to add 10% more protein in lieu of 10% of carbohydrates to represent a Mediterranean Diet; there was no allowance made for fat, which was still ultra-low. This isn’t really representative of true, traditional Mediterranean diets which are replete with fat from olive oil, nuts, fatty fish, poultry, lamb, and full-fat cheese, butter and yogurt.
To mimic a low-carb diet, they added 10% of calories from fat, reducing carbohydrates by 10%. But that left the “low-carb” diet with a whopping 48% of calories from starches and sugars! And all the added fat came from polyunsaturated sources, because apparently the study authors felt that the addition of even a smidgeon of saturated fat or cholesterol would pose unacceptable risks to the research subjects.
So you have a comparison of three “healthy” diets, consisting of roughly 58% carbs/15% protein/27% fat (DASH); 48%/25%/27% (“Mediterranean”); 48%/15%/37% (“Low-carb”).
In fact, “In all three diets, breads (both white and wheat) and rolls contributed 44% to 55% of total grains. This was followed by pasta, rice, and hot breakfast cereals (18% to 21%) and ready-to-eat cereals (9% to 10%).” And “Tropical fruits such as bananas, and temperate-climate fruits such as dried apricots, pears, apples, and peaches, were common in all three diets.”
Why such a timid diet modification? Could it be that the researchers were philosophically moored to the standard hospital-approved DASH diet? They conjure images of early explorers, before the age of Columbus, who dared not sail too far from familiar shores lest they fall off the end of the flat earth.
How do these experimental diets represent the real-world circumstances of the millions of strivers who leverage very low-carb diets (less than 10%) to successfully reverse obesity, insulin resistance, Type 2 diabetes, adverse cholesterol ratios, and inflammation, and thereby lower cardiovascular risk? And why is the study predicated on the now discredited notion that saturated fats and cholesterol (and not carbohydrates) are the true drivers of cardiovascular risk?
In psychology, they call it confirmation bias. Wikipedia defines it as: “the tendency to search for, interpret, favor, and recall information in a way that affirms one’s prior beliefs or hypotheses. It is a type of cognitive bias and a systematic error of inductive reasoning. People display this bias when they gather or remember information selectively, or when they interpret it in a biased way. The effect is stronger for desired outcomes, emotionally charged issues, and for deeply entrenched-beliefs.”
And how is it that it emanated from a prestigious institution like Harvard?
Study author Dr. Stephen Juraschek arrives at a completely unwarranted conclusion:
“There are multiple debates about dietary carbs and fat, but the message from our data is clear: eating a balanced diet rich in fruits and vegetables, lean meats, and high in fiber that is restricted in red meats, sugary beverages, and sweets, will not only improve cardiovascular risk factors, but also reduce direct injury to the heart. Hopefully, these findings will resonate with adults as they shop in grocery stores and with health practitioners providing counsel in clinics throughout the country.”
No, they won’t, because your study doesn’t support those inferences!
Underlying pronouncements like these is a cynical calculus—that Americans, like unruly children, can’t be coaxed into adopting too stringent a dietary discipline.
It’s my opinion that purveyors of dietary “truth” like this suffer from an excess of moderation; their timidity discourages the public from taking bold transformational steps via such proven strategies as Paleo or Keto diets or intermittent fasting to slash their cardiovascular risk. Studies like this may inspire Americans to take “baby steps” toward improving their food choices, but minimizing the criticality of macronutrient ratios is a disservice to discerning consumers of health information in search of practical strategies to avert the leading diet-related causes of death in the U.S.
Though we think of declining estrogen as the hallmark of menopause, it's actually common for…

Up to 12 percent of Americans have ulcers at some point in life. Peptic ulcers…
Gallbladder disease is a modern illness. An estimated 20 million Americans have gallbladder disease. The…

Q: My husband suffers from generalized anxiety disorder (GAD). He has been on antidepressants for…
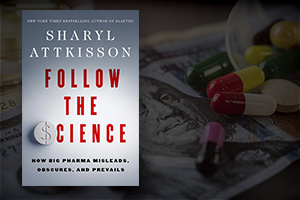
I recently had the opportunity to interview Sharyl Attkisson about her new book Follow the Science. Attkisson is…

Q: Is it ever a good idea to give insulin to a type 2 diabetic…

Leyla Weighs In: Navigating Teen Health in the Digital Age

Our virtual voicemail is open 24/7, so there's no need to wait to submit your questions for Dr. Hoffman. Leave a message, and you may hear your question featured on the Intelligent Medicine radio program!