



| By Dr. Ronald Hoffman
You may have never heard of it, but it’s so prevalent, chances are that you or someone you know suffers from it. Alcohol and hepatitis C used to be the main reasons why people ended up with cirrhosis and liver failure requiring transplantation, but non-alcoholic fatty liver disease (NAFLD) is rapidly catching up.
First recognized in the 1980s, NAFLD is becoming one of the most common liver diseases in affluent countries. The prevalence of NAFLD in the general population ranges from 20% to 30% in Europe and is as high as 46% in the United States.
Its rise mirrors the soaring incidence of metabolic syndrome, obesity and type 2 diabetes in the West. Because it’s not readily diagnosed, it is claimed that its prevalence is vastly underestimated.
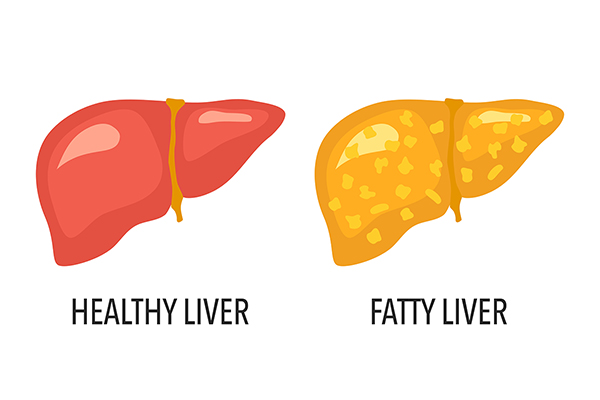
A normal liver is brown and uniform in consistency. In NAFLD, it becomes enlarged and infiltrated with yellowish fat. With time, inflammation causes fibrosis—lacing with hardened scar tissue. Eventually, functional liver tissue is displaced with nodular accumulations of fibrotic tissue, causing cirrhosis, and liver failure ensues. Hepatocellular carcinoma can also develop.
The only definitive cure for cirrhosis is liver transplantation, and patients with NAFLD—who often have comorbidities of obesity, diabetes, and heart disease—don’t fare well. During the past 10 years, the prevalence of NAFLD as an indication for liver transplantation has increased by 170%. During the same period, hepatitis C virus (HCV) and alcoholic cirrhosis as a reason for liver transplantation only increased by 14% and 45% respectively.
Elevated liver function tests (AST and ALT) are suggestive of NAFLD, but the only definitive test is a right upper quadrant ultrasound that reveals abnormalities in the consistency of the liver indicating fat infiltration. A relatively new ultrasound test called the FibroScan can delineate how extensively the hardening of fibrosis has progressed.
Diet is the main culprit in NAFLD. Geese raised for pâté de foie gras (literally “pâté of fatty liver”) provide a graphic animal model for NAFLD. In a controversial practice called gavage, they are force-fed carbohydrates in the forms of corn meal and white bread prior to slaughter. The human implications are inescapable.
In fact, the chronology of the epidemic of NAFLD closely parallels the popularization of the ubiquitous sweetener high fructose corn syrup in the 1980s—which also tracks with our dramatic decades-long uptick in obesity and metabolic syndrome. It’s been theorized that fructose is uniquely harmful to the liver. In a review entitled “Fructose and NAFLD: The Multifaceted Aspects of Fructose Metabolism”, researchers conclude that fructose, by virtue of a panoply of harmful effects “appears as one major factor not only of the initiation of hepatic steatosis, but also of its progression to NASH and more severe stages of the disease.”
Because of the ubiquity of NAFLD, BigPharma is hot on the trail of potential block-buster drugs to reverse it—so far with no luck. But in my experience, it’s only natural interventions that can reliably reverse NAFLD:
Diet: It’s essential to follow a very low-carb diet to alleviate NAFLD. Paradoxically, even diets delivering significant amounts of fat, while restricting carbs, like the keto diet, have demonstrated success in reversing fatty liver. A recent study showed the Mediterranean diet—rich in fiber, polyphenols and polyunsaturated fat—helped curb NAFLD. A recent trial showed that 12 weeks of olive oil consumption alleviated the severity of fatty liver.
A consistent theme is that even moderate weight loss of just 3-5% of total body mass has beneficial effects on liver histology.
An interesting sidebar: Patients with celiac disease experience more NAFLD, providing even more impetus to ditch bagels and croissants.
What to drink: Avoid sugary drinks and soda—studies confirm their link to NAFLD. Alcohol, per its deleterious effects on liver, is a no-no. But coffee—even the caffeinated kind—seems beneficial.
Exercise: Logically enough, exercise, because of its effects on metabolism, has been shown to be helpful for NAFLD. But the surprise is that, even apart from its impact on weight loss, exercise helps rid the liver of fat. Studies suggest that aerobic exercise and strength training have equivalent benefits for NAFLD.
Fresh air: Some new-think on NAFLD contends that particulate matter and nitrogen dioxide in the air can worsen NAFLD.
Vitamins and minerals: There are some do’s and don’ts. Many vitamins and minerals have antioxidant and anti-inflammatory effects, so adequacy is essential. But avoid excess niacin and vitamin A (the retinol kind); a surfeit of either can have deleterious effects on the liver.
There’s some evidence ample vitamin D helps NAFLD. Vitamin E has been used in clinical trials to treat NAFLD, and tocotrienols have shown promise in a recent review.
Betaine: Also called trimethylglycine (TMG), betaine has proven helpful in an animal model of NAFLD.
Choline: In a large sample of US adults, higher dietary choline was associated with a lower risk of NAFLD.
Milk Thistle: Silymarin is an extract from the milk thistle plant. Many studies have demonstrated its beneficial effects in a variety of liver conditions. In one study lasting 48 weeks, a significantly higher proportion of NAFLD patients in the silymarin group had reductions in fibrosis.
Probiotics: The liver is directly connected to the intestines via the portal vein; endotoxins generated by dysbiosis within the microbiome have a harmful impact on liver function. Accordingly, a recent review suggests that “supplementation with probiotics in the management of NAFLD/NASH seems to be a practical therapeutic strategy.”
Berberine: Once purified from goldenseal, most is now sourced more sustainably from Oregon grape root. It’s an alkaloid that shows promise in reversing metabolic syndrome. A 2022 review concluded that “the complex and diverse pharmacological effects of berberine, such as regulation of lipid and glucose metabolism and increased insulin sensitivity, may elucidate its promising role in the treatment of NAFLD.”
EGCG: A catechin prominent in green tea, EGCG has proven effective in a mouse model of NAFLD. On the other hand, excess EGCG has been implicated by some reports as a cause of liver damage. The key may lie in a genetic variation that confers susceptibility to a minority of people.
Curcumin: Like EGCG, curcumin’s anti-inflammatory properties have been shown helpful for NAFLD, while at the same time occasionally prompting rare incidents of liver damage.
Aged Garlic Extract: Like a Swiss Army knife, aged garlic extract keeps delivering: A recent study demonstrated “Aged garlic extract ameliorates fatty liver and insulin resistance and improves the gut microbiota profile in a mouse model of insulin resistance.”
CLA: A trans-fat that’s healthy? Conjugated linolenic acid is found naturally in dairy products. A study in mice concluded “CLA potentially contributed to ameliorating hepatic steatosis in obese mice via modulating liver inflammation, intestinal permeability, and gut microbiota, which suggests CLA is more suitable for people with obesity or overweight.”
Bergamot: An extract of citrus, bergamot is responsible for the distinctive fragrance of Earl Grey tea. Best known for its cholesterol-lowering benefits, lately it’s been touted as a treatment for NAFLD.
Resveratrol: There’s some potential vs. NAFLD, but not enough to justify guzzling Pinot Noir; stick to supplements if you have liver disease.
NAC: A generator of the body’s master antioxidant glutathione, N-acetylcysteine has proven efficacy even in acute liver failure caused by Tylenol overdose. Studies have demonstrated NAC’s ability to normalize liver function, reduce inflammatory markers and curb fibrosis in patients with NAFLD.
Nicotinamide riboside: A mitochondrial support formula containing nicotinamide riboside (NR), L-serine, N-acetyl-L-cysteine (NAC), and L-carnitine tartrate was found in a human trial to significantly decrease liver fat by 10% and improve liver function. Animal studies have confirmed NRs potential to ameliorate NAFLD.
Though we think of declining estrogen as the hallmark of menopause, it's actually common for…

Up to 12 percent of Americans have ulcers at some point in life. Peptic ulcers…
Gallbladder disease is a modern illness. An estimated 20 million Americans have gallbladder disease. The…

I just returned from a dive trip to Turks and Caicos and wanted to share…

Q: According to my latest bloodwork, I have low levels of ferritin. Can you shed…
Dr. Antonio Bianco, recipient of the American Thyroid Association’s John B. Stanbury Thyroid Pathophysiology Medal,…

ENCORE: Q&A with Leyla, Part 1: Selfies and Plastic Surgery

Our virtual voicemail is open 24/7, so there's no need to wait to submit your questions for Dr. Hoffman. Leave a message, and you may hear your question featured on the Intelligent Medicine radio program!