A controversy has been brewing in the medical world over “overdiagnosis.” In fact, Overdiagnosed: Making People Sick in the Pursuit of Health is the title of a book by H. Gilbert Welch, MD, professor of Medicine at the Dartmouth Institute for Health Policy & Clinical Practice.
The book is described as follows:
“A complex web of factors has created the phenomenon of overdiagnosis: the popular media promotes fear of disease and perpetuates the myth that early, aggressive treatment is always best; in an attempt to avoid lawsuits, doctors have begun to leave no test undone, no abnormality overlooked; and profits are being made from screenings, medical procedures, and pharmaceuticals. Revealing the social, medical, and economic ramifications of a health-care system that overdiagnoses and overtreats patients, Dr. H. Gilbert Welch makes a reasoned call for change that would save us pain, worry, and money.”
In 2012, I tackled the issue of “Pre-Disease” in an article for the journal Clinical Advisor. I concluded that there were both upsides and downsides to early forecasting of increasing numbers of medical conditions.
No question we are in the midst of an epidemic of overdiagnosis. Rates of medication for kids with ADD/ADHD are soaring. We are detecting breast cancer and prostate cancer earlier than ever, but the value of screening tests like routine mammograms and PSAs has come under fire.
We are also widening the net for statin prescribing with ever-more lenient thresholds for eligibility. Curious about my own status as a healthy 64-year-old triathlete who is not overweight, without diabetes, hypertension, smoking, or a family history of heart disease—the traditional risk factors—I used a plug-in at www.cvriskcalculator.com to assess whether I was a candidate for statins.
Amazingly, after filling out a perfunctory on-line questionnaire, my print-out informed me:
“On the basis of your age and calculated risk for heart disease or stroke over 7.5% [It’s 8.5%] the ACC/AHA guidelines suggest you should be on moderate to high intensity statin.”
This is balderdash. But it illustrates how a widening net of overdiagnosis is inappropriately categorizing too many Americans as potential lifetime customers for BigPharma.
Pre-diabetes is in the cross-hairs as another instance of overdiagnosis. What is the definition of pre-diabetes?
In 2010, the American Diabetes Association (ADA) set aside the obsolete guideline that defined diabetes as a fasting blood sugar of greater than 126. This, of course, was an imprecise way of detecting abnormal sugar metabolism, because a high percentage of patients without fasting glucose >126 have non-insulin-dependent diabetes.
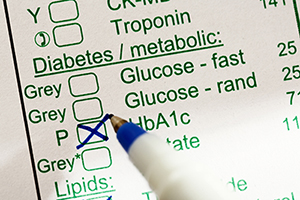
Fasting blood sugar was replaced with hemoglobin A1c, a measurement of the average response of hemoglobin to elevated blood sugar over 120 days—a metric superior to a single blood sugar determination.
The ADA defines diabetes as hemoglobin A1c of 6.5% or greater.
The controversy over “pre-diabetes” arose in 1997, when the ADA first proposed that individuals with “impaired fasting glucose (IFG)” of 100 to 126 are candidates for the diagnosis of intermediate levels of glucose elevation that are out of the range of normal but have not yet reached diagnostic levels for diabetes, i.e. prediabetes. This translates to a hemoglobin A1c in the intermediate range of 5.7% to 6.4%.
This immediately triggered push-back from some health authorities who argued that IFG by no means portends an inevitable progression to frank diabetes, and that by so categorizing an enormous segment of the population, we might put people at risk for unnecessary worry and over-aggressive treatment, with its attendant side effects and expense.
In fact, a recent study found that more than half of older adults with multiple medical conditions may be over-treated with diabetes drugs. This puts them at risk for dangerous episodes of low blood sugar and other complications.
A recent article in the Wall Street Journal entitled “Pre-diabetes Awareness Campaign Sparks Pushback” details the controversy.
The Centers for Disease Control estimates that of the 1 in 3 Americans who have prediabetes, the majority are unaware of it.
Therefore, Matthew Peterson, the managing director of medical information and professional engagement of the ADA states: “We’ve proven [pre-diabetes] is an intervention time. It’s a call to action.”
In 2014, the U.S. Preventive Services Task Force urged that all adults over 45 be screened for diabetes and impaired fasting glucose.
But in an article in the British Medical Journal, Dr. John Yudkin claims that the diagnosis of pre-diabetes casts too wide a net. He estimates that by the ADA criteria, over one-half of the population of China would be considered prediabetic. Additionally, the value of rigorous medical management of pre-diabetes with existing drugs has not been established. He argues “A label of pre-diabetes brings problems with self image, insurance, and employment as well as the burdens and costs of healthcare and drug side effects.”
I disagree. I have a strong opinion on the issue of screening for pre-diabetes. While, as in the statin example above, I’m concerned about drug companies leveraging screening programs into marketing bonanzas for their medications, awareness of pre-diabetes provides a “teachable moment” for patients to undertake lifestyle change. The British Medical Journal comments:
“Far from turning healthy individuals into or labeling them ‘patients’ and pathologizing their health status, prediseases ought to be seen in the context of prevention and that their management and control, as with the prevention of hypertension, diabetes and obesity, is behavioral, non-pharmacologic and not confined to the clinic.”
The problem with the critics of prediabetes awareness is that they are thinking too narrowly in terms of interventions. They think that all we have to offer patients are drugs, which they acknowledge are limited in efficacy and fraught with side effects.
On the other hand, the power of a low-carb diet, accompanied by aerobic exercise and strength training, is undeniable. In what I once dubbed “The ‘Duh’ Story of the Year” it was reported in 2015 that “Diet and exercise are effective in preventing type 2 diabetes, task force finds.” Along with certain supplements, I’ve been able to normalize blood sugars for the vast majority of my non-insulin dependent diabetics—providing patients are sufficiently motivated to comply.
And there’s motivation aplenty. Pre-diabetes, even when it doesn’t progress to full-blown diabetes, is a recognized risk factor for heart disease, stroke, dementia, and many cancers. It promotes inflammation and impairs immune response and wound healing. And even in the absence of sky-high blood sugars, it may predispose to the nerve, eye and circulatory problems that plague true diabetics.
NOTE: Over-reliance on the hemoglobin A1c score could be a trap. Until recently, I was puzzled by a spate of apparently healthy patients who had borderline or high hemoglobin A1c despite their best efforts at diet and exercise. Many lacked the typical metabolic syndrome features of excess belly fat and high triglycerides.
The puzzle was solved when it was revealed that for patients with iron deficiency, hemoglobin A1c may be falsely elevated. Therefore, if your doctor diagnoses you with pre-diabetes on the basis of the hemoglobin A1c test alone, be sure to remind him or her to check your iron and ferritin levels.
If you haven’t yet had your hemoglobin A1c checked, there’s a free screening test you can take at www.DoIHavePrediabetes.com. Based on your family history, height, weight, race, blood pressure, exercise level, sex and age, the algorithm yields a rough prediction of your risk for prediabetes. If your score turns out to be high, print a copy and take it to your doctor for further evaluation.
And don’t rest assured with a bland dismissal from your doctor that “it’s normal for older people to have slightly high blood sugars.” You can improve your health and prospects for longevity by optimizing your scores into the normal range (5.7% or less).
If you want an even more sensitive predictive test for prediabetes, consider a three or four hour glucose tolerance test with not just glucose determinations, but also with insulins. An abnormally high insulin response to a sugar challenge predicts prediabetes well before elevated blood sugars and even hemoglobin A1c emerge. It’s a test that I’ve found invaluable for inspiring early corrective action by patients.
Check out this week’s podcast with Dr. Michael Murray, where we discuss this very topic! You can listen here: Diabetes Prevention and Reversal