Do you have allergies? Sneezing, wheezing, burning eyes, or flushing, itchy skin with hives? Do certain foods trigger stomach cramps or diarrhea? Or do you suffer from frequent headaches or migraines, bouts of nausea, severe menstrual cramps, or panic attacks characterized by a racing heart?
You’ve dutifully tried allergy shots—sometimes for years!—to no avail. Antihistamines work for you, but only partially. Food allergy tests keep coming up negative. There seem to be no clear dietary precipitants—your food reactions seem to be all over the map. But your doctor insists your allergy blood tests and skin tests don’t come up positive for foods. Still, you try popular gluten-free, dairy-free or candida diets, but they only make minor dents in your symptoms.
The answer may lie in a new understanding of something called histamine intolerance. Histamine, of course, is what antihistamines are supposed to suppress. Histamine is part of our bodies’ natural response to insults or invaders. It prompts blood vessels to swell and fluid to leak from capillaries, causing swelling. Think of the itching you get at the site of a mosquito bite, in response to the foreign proteins deposited by the insect’s saliva.
Histamine intolerance is actually a “pseudo-allergy,” which is why it’s not picked up by conventional allergy blood tests that measure IgE. It results when histamine levels soar in the body.
To use a bathtub analogy, there are two ways a tub can overflow: 1) If the faucet is turned on too high, or 2) If there’s a stopper in the drain. It’s the same with your body. If either occurs, or both simultaneously, your allergy “tub” can overflow, resulting in symptoms of histamine overload.
The discovery of an enzyme called diamine oxidase (DAO) has helped to unlock the key to histamine intolerance. DAO is normally present in the intestine to control excess histamine. It acts to break down histamine in the gut.
Research indicates that certain individuals are genetically prone to low levels of DAO. It can be measured via a blood test, but requires processing by specialty labs that are not licensed in certain states. More readily available are blood tests that can reveal high levels of histamine, presumably resulting from insufficient DAO activity.
To summarize—and it gets a little complicated here, so bear with me—there are 6 ways that foods can send your histamine past the threshold where you experience allergic symptoms:
- The old fashioned way—a direct measurable food allergy, say to casein from dairy (to return to the bathtub analogy, “faucet”).
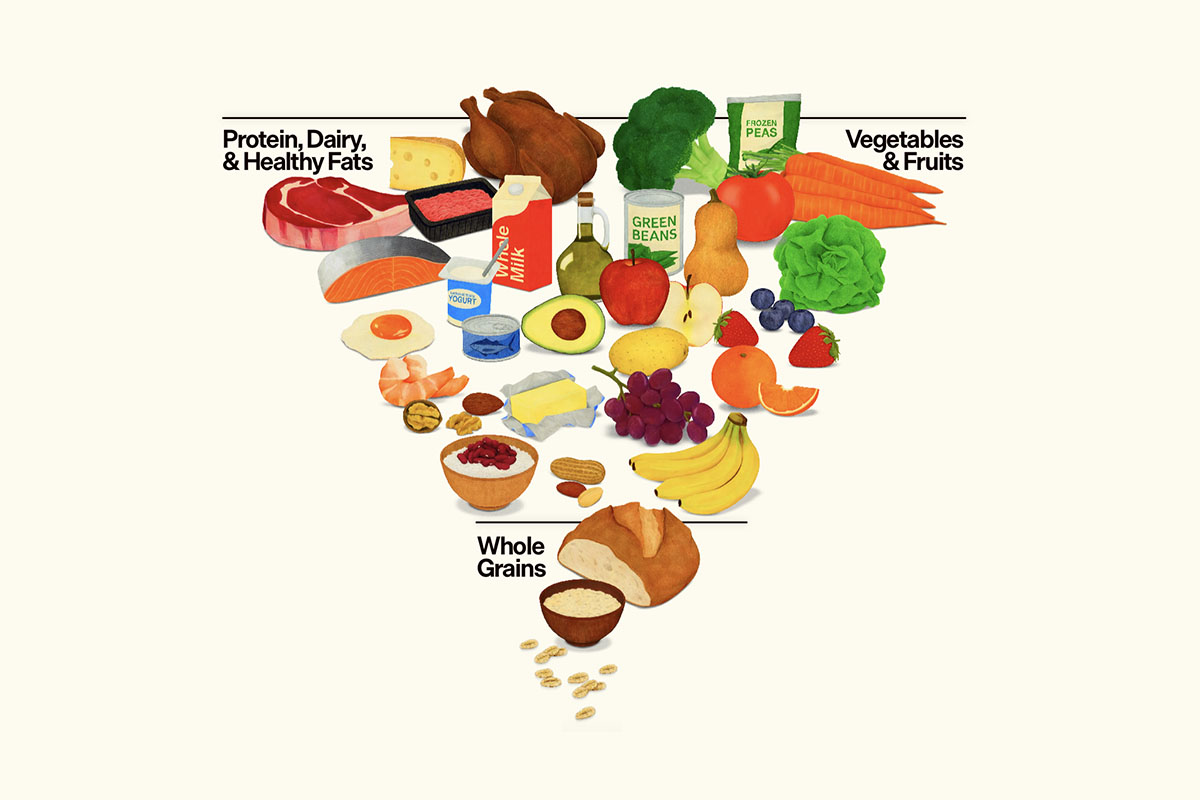
- Foods that are rich in histamines (“faucet”). These include alcohol (especially red wine), aged meats; shellfish or spoiled fish; fermented products like sauerkraut, soy sauce, Worcestershire sauce, yeast extracts and vinegar; and beans and pulses.
- Foods that are rich in biogenic amines, which don’t directly trigger allergies, but compete with histamine for degradation by DAO (“stopper”). These include pineapple; bananas; raspberries; peanuts and wheat germ.
- Other foods that don’t contain histamine but trigger mast cells to release histamine (“faucet”). These include fruits like kiwi, lime, lemon, pineapple, papaya and plum; additives like MSG, sulfites, benzoate, nitrites and artificial food dyes; and tomatoes.
- Foods or beverages that inhibit DAO (“stopper”): Alcohol; black, green and mate tea.
- Foods that can cause “leaky gut” (“faucet”). They make the intestines leak, allowing passage of histamine or macromolecules from food into the body, triggering IgE or IgG food allergies. These include alcohol and hot spices like chili peppers.
Finally, certain commonly-used medications inhibit DAO (stopper): These include Elavil, Tagamet, NSAIDs, aspirin, aminophylline, Reglan, verapamil, and Moduretic.
Can you be “allergic” to your own hormones? Many women report a surge in their symptoms of bloating, diarrhea, nasal congestion and wheezing corresponding with their periods—not to mention intense menstrual cramps.
This may not be coincidental. Histamine has been shown to enhance the production of estradiol, making women feel more “hormonal”; conversely, higher levels of estrogen can potentiate the action of histamine, exacerbating allergy symptoms including premenstrual headaches and migraines.
Interestingly, production of DAO by the placenta in pregnancy soars by as much as 500-fold; increased DAO pulls the stopper on excess histamine accumulation. This may explain, in part, why pregnant women often enjoy a temporary respite from allergies.
So what are the practical consequences for you?
If you have symptoms of histamine intolerance (nasal congestion, asthma, hives, headaches, abdominal cramps, diarrhea, etc.);
And your symptoms are partially relieved by antihistamines, or brought on by consumption of any of the above histamine-releasing or DAO blocking foods or medications;
Or, if you’re a premenopausal woman, and your allergic symptoms seem worse at certain times of the month;
Or, your blood tests show high levels of histamine or low levels of DAO;
You should:
- Redouble your efforts to avoid histamine-boosting foods
- Avoid DAO-blocking drugs
- Use natural anti-histamines (C, B6, quercetin)
- Take DAO with each meal
Most importantly, seek professional guidance from a health practitioner well-versed in histamine intolerance. Other medical problems can mimic histamine intolerance, and sometimes need to be ruled out before simply following the protocol outlined above. It’s early in our understanding of the complex phenomenon of histamine intolerance, and we’re only just now refining our approach to this challenging disorder. But its discovery finally spells hope for many patients afflicted with a bewildering array of symptoms
Additional Resources:
Maintz L and Novak N, “Histamine and histamine intolerance”, Am J Clin Nutr 2007;85:1185-96http://ajcn.nutrition.org/content/85/5/1185.long
DAO inhibitor www.histame.com
http://www.histamineintolerance.org.uk
http://www.histamine-intolerance.info