This month marks the publication of the first study that conclusively documents the benefits of diet for treating depression. Researchers love acronyms, so they contrived to call it the SMILES trial—“Supporting the Modification of Lifestyle in Lowered Emotional States.” Here’s a contrasting acronym: SAD which stands for “Standard American Diet.”
The use of diet and supplements in support of the treatment of depression and anxiety is hardly something novel. Roger Williams Ph.D. wrote A Physician’s Guide to Orthomolecular Medicine in 1977, containing the works of such pioneers as Abram Hoffer and Linus Pauling. It’s a book I found profoundly influential in medical school and in my early career.
Subsequently I’ve seen countless patients with depression and anxietywhose symptoms have been alleviated with nutrition. It’s hardly surprising, since the majority of sufferers of emotional disorders have abysmal diets. They don’t have the wherewithal to shop or prepare good food, and they crave “comfort foods” laden with sugar and poor quality fats. Often, they lack critical nutrients like B vitamins, vitamin D, magnesium, amino acids and Omega 3s. Poor nutrition and depression create a self-reinforcing vicious cycle.
SMILES was a 12-week trial in which 67 patients with major depression—the kind that doesn’t respond readily to medication or psychotherapy—were divided into two groups.
One group got intensive dietary counseling consisting of seven sessions with a clinical dietician. They were told to adopt a modified Mediterranean diet. In the words of the study authors:
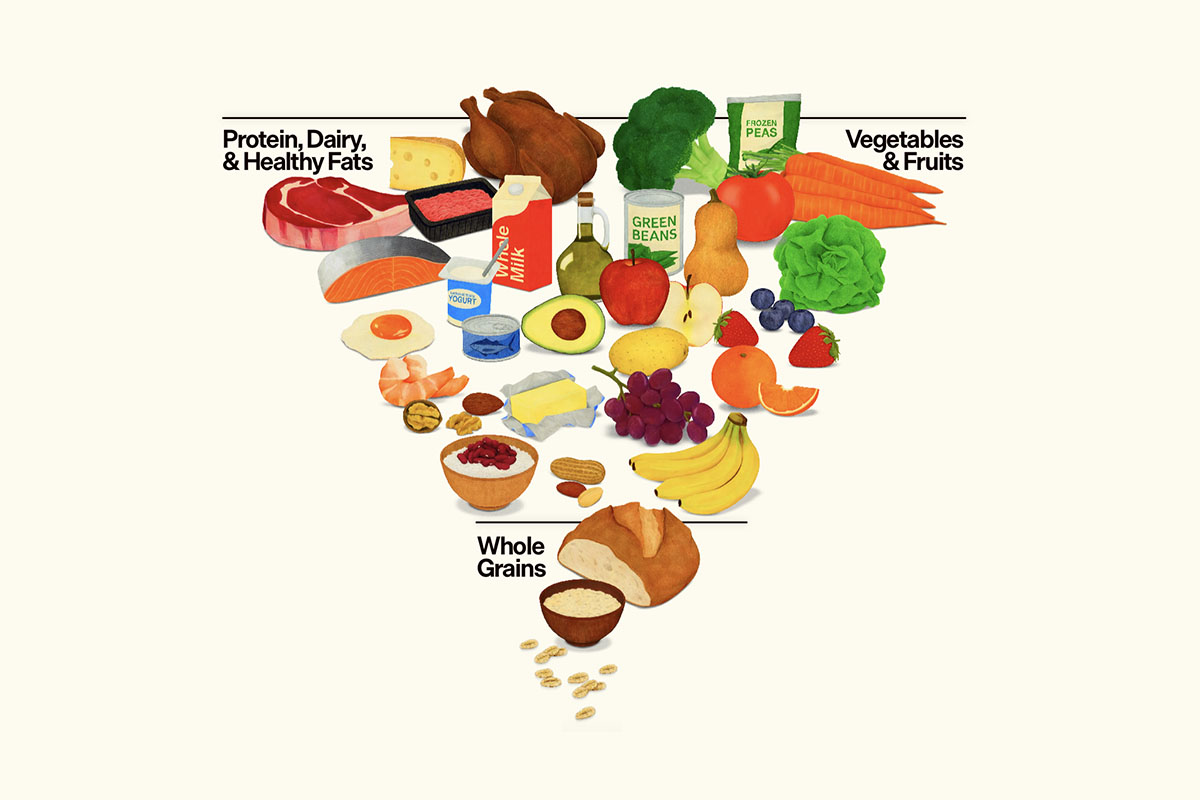
“The primary focus was on increasing diet quality by supporting the consumption of the following 12 key food groups (recommended servings in brackets): whole grains (5–8 servings per day); vegetables (6 per day); fruit (3 per day), legumes (3–4 per week); low-fat and unsweetened dairy foods (2–3 per day); raw and unsalted nuts (1 per day); fish (at least 2 per week); lean red meats (3–4 per week), chicken (2–3 per week); eggs (up to 6 per week); and olive oil (3 tablespoons per day), whilst reducing intake of ‘extras’ foods, such as sweets, refined cereals, fried food, fast-food, processed meats and sugary drinks (no more than 3 per week). Red or white wine consumption beyond 2 standard drinks per day and all other alcohol (e.g. spirits, beer) were included within the ‘extras’ food group. Individuals were advised to select red wine preferably and only drink with meals. The dietary composition of the ModiMedDiet was as follows: protein 18% of total energy (E); fat 40% of E; carbohydrates 37%”
As you may notice, this diet was not particularly stringent; it permitted grains, dairy foods, legumes, and even offered leniency with regard to small amounts of sugary beverages, alcohol, sweets and fast foods. It didn’t even include much Omega 3-rich fish. The goal, apparently, was modest harm reduction in an effort to assure better adherence to realistic goals. Had patients followed a more committed Paleo-style diet, for instance, as have some of my patients who’ve successfully battled depression, perhaps the improvements would have been even more spectacular.
Additionally, the SMILES trial did not evaluate the efficacy of supplements and nutraceuticals vs. depression. Imagine the benefits that might have been attained with targeted supplementation!
How do you provide a “placebo” to control for the effects of all that attention provided to the research subjects? Control patients who did not receive the diet intervention were given social support counseling for an equivalent number of sessions.
SMILES did not aim to supplant conventional therapy with diet counseling. 55 of 67 patients were taking medication and/or undergoing psychotherapy. So this is not alternative medicine—it’s integrative or complementary medicine, combining both conventional and natural interventions. As we’ll see, it turned out to be intelligent medicine.
At the beginning of the study and again at its conclusion after 12 weeks, each patient was given a battery of standard tests that are acknowledged by psychiatric professionals to gauge the depth of depression. The SMILES diet group achieved remission from depression at a rate of 32.3%. By contrast, only 8% of the SAD diet group achieved remission.
This adds up to an NNT (number needed to treat) of 4.1. That means that 4 depressed patients would have to undergo the diet intervention for one to achieve remission. While that may not sound impressive, bear in mind that many drugs have NNTs that are in the mid-to-high double digits. For example, statins have an NNT of 50-100 in terms of preventing heart attacks. A new depression drug with an NNT of 4.1 would be hailed as a breakthrough, would receive accelerated approval from the FDA, and reap billions for the pharmaceutical industry!
The authors conclude: “These results indicate that dietary improvement may provide an efficacious and accessible treatment strategy for the management of this highly prevalent mental disorder.” They add, parenthetically, that the diet might yield additional benefits by relieving other physical ailments of depression sufferers.
Why should a healthier diet fight depression? There are multiple reasons:
- It’s anti-inflammatory. We recently did a podcast on the benefits of an anti-inflammatory diet with Dr. David Seaman, author of The DeFlame Diet. It’s often overlooked that the brain is part of the body, and when you suffer from systemic inflammation, your brain metabolism might be impaired, resulting in altered mood. We see this clearly in rheumatoid arthritis, colitis, and lupus. Merely losing extra body fat attenuates inflammation. The dietary components that are most pro-inflammatory are sugar, refined carbohydrates, and vegetable oils. They permeate the junk foods that make up the SAD diet. By contrast, the Omega 3 oils, plant polyphenols, and herbs that are mainstays of the Mediterranean diet are anti-inflammatory.
- It gets you off the blood sugar roller coaster. When you’re “hangry,” it’s not the time to reach for a Snickers bar for a quick fix. Your blood sugar will soar transiently, only to plummet minutes later, perpetuating a vicious cycle of craving and binging. A high percentage of patients with depression are not just hypoglycemic, they’re insulin-resistant. “Type 3 diabetes”—insulin resistance in the brain—has been identified as a cause of mood disturbance and cognitive impairment when the brain’s energy production is compromised.
- It’s rich in vitamins and minerals. Plant foods provide magnesium, and animal protein is rich in iron, B vitamins, and the amino acids.
- It’s a source of Omega 3s. Nuts and fish provide Omega 3 fatty acids like linolenic acid, EPA, and DHA which are natural anti-depressants
- It offers sufficient protein. In several recent studies, it was found that a vegetarian diet was associated with higher risk for depression. Part of the problem may be the lack of readily utilizable protein due to a dearth of animal products. Amino acids are essential building blocks for feel-good neurotransmitters.
- There may be microbiome effects. We are increasingly aware that a brain-gut connection exists. Studies suggest that probiotics may alleviate anxiety and depression. Adequate prebiotic dietary fiber is necessary to cultivate healthy intestinal flora. The SAD diet is almost bereft of soluble fiber, and is laden with artificial sweeteners, preservatives and emulsifiers which damage the microbiome.
From the foregoing, it should be obvious that nutrition is an essential adjunct to treatment of depression. Not that it’s a panacea; in an integrative workup, we assess many factors, not just nutritional status. A patient’s depression might be the result of hypothyroidism, adrenal stress, menopause, or andropause. Hormone replacement can be critical. Alternatively, conditions like Lyme disease, viral infections, chronic sinusitis, sleep disorders, heavy metal toxicity, or allergies might be contributory.
But the SMILES trial is a clarion call for educating health professionals about the benefits of basic nutritional therapy for mood disorders. I get many referrals from psychologists and therapists who feel their patients need an added dimension of care in addition to talk therapy or medication. I strongly believe that it’s high time that every patient suffering from depression undergo a trial of diet change, if not a full program of targeted nutritional supplementation.