Suffering from office or classroom brain-fog? You’ve heard of “sick building syndrome”. It’s a recognized threat to health, affecting as many as 30% of indoor environments. According to the Environmental Protection Agency, “Building occupants complain of symptoms such as cough; chest tightness; fever, chills; and muscle aches.” In an embarrassing episode, numerous employees at EPA headquarters in Washington were found to be suffering from it in 1988.
Now Harvard researchers have confirmed that indoor air quality can have a significant impact on employees’ cognitive function. Perhaps that explains your recurrent mid-afternoon crash if you’re an office worker or a student. And you thought it was that heavy lunch!
The COVID era has reminded us that air circulation is poor in energy-efficient homes, workplaces, and classrooms. Viral particles are trapped inside. So, too, are chemicals, and carbon dioxide (CO2). It was found that even modest increases in CO2 impaired response time and performance in experimental subjects. When people are cooped up in stuffy rooms, their exhalations cause CO2 levels to soar.
This prompts us to recall a recent study in JAMA which assesses levels of carbon dioxide in children wearing different types of masks. Especially in small children, it was found, exhaled breath was sufficiently trapped inside restrictive masks to result in CO2 levels “higher than what is already deemed unacceptable by the German Federal Environmental Office by a factor of 6.”
The study raised a firestorm and was ultimately retracted. It was claimed that the authors’ methods were sketchy, and their conclusion that masking kids could be harmful was unwarranted. So masking of small kids continues apace.
Whatever the merits of the study, it’s a no-brainer that kids and adults need fresh, clean air, free of accumulated viral particles. The simplest solution is to reconfigure our buildings and schools to permit open windows, and to install air filters and smart HVAC systems. And get rid of all that plexiglass—studies show it actually impedes air circulation.
Should you worry if you don’t have a reaction when you take the COVID vaccine? I recently visited a relative who is 93. I asked her how she felt after her shots. She said, “Oh, it was like nothing, it didn’t bother me at all.” I then turned to her caregiver—36—who had gotten the same series of shots with her on the same days. “I didn’t feel right for two weeks, it’s only now that I’m feeling better.”
When patients tell me of very sore arms, or fever to 101, or achy body, I’ve been tempted to reassure them that that’s a good sign: “It means you’re having a strong response because you have a healthy immune system. You’re likely to get more protection than someone who barely notices they got the shot.”
A recent study tackled that question with a surprising result: severity of reactions was not a predictor of vaccine-induced antibodies one month after immunization.
206 health care workers at the Walter Reed Medical Center received the two-shot Pfizer vaccine and their reactions recorded. It was found that younger and thinner recipients had worse symptoms, and they were more pronounced in women. (Maybe smaller people need smaller doses?) Nevertheless, one month after getting the shots the participants’ vaccine-induced antibodies weren’t different.
So lack of vaccine response did not equate to less protection.
Keep in mind this is a preliminary study, of short duration, and it was based on a blood assessment of immunity rather than a recording of actual breakthrough infections which might emerge only months later. But it may provide some measure of reassurance for those out there who had so little reaction they suspect they were injected with a dud vaccine, or have impaired immunity. Feeling crappy is not mandatory for protection.
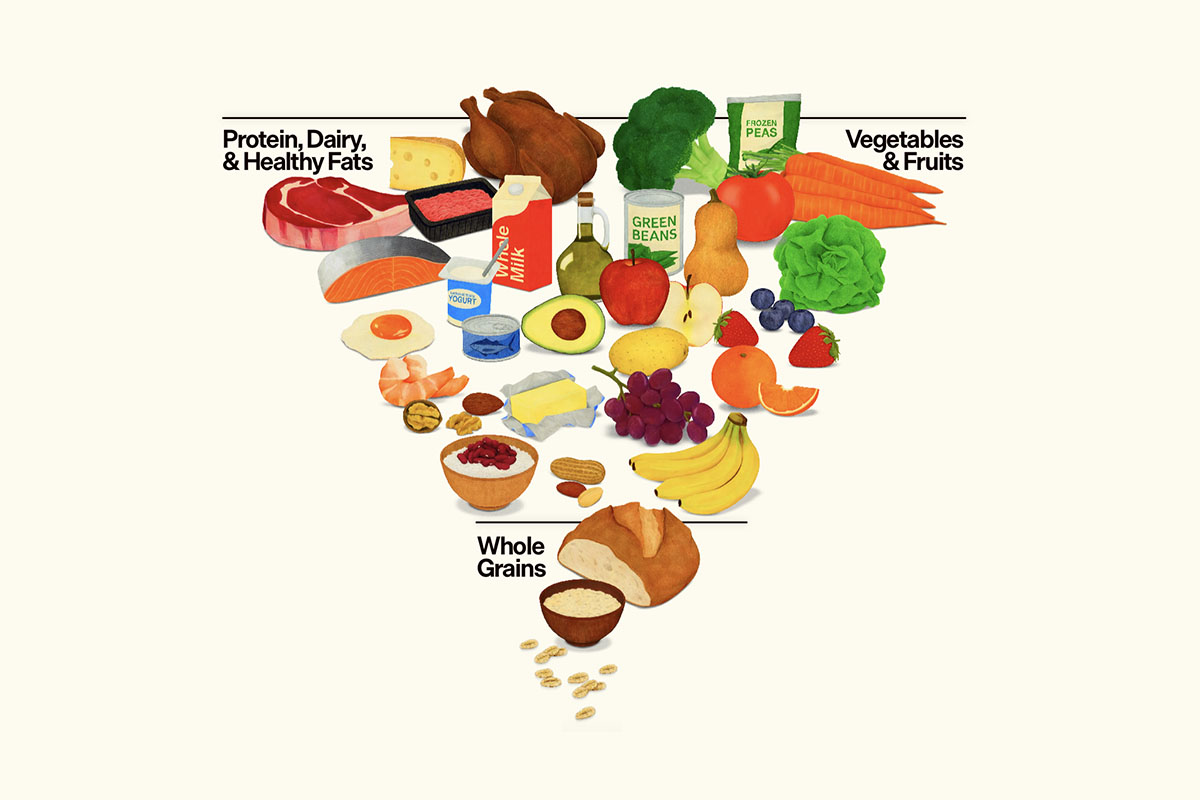
Nuts and avocados: Three new studies offer good news for healthy food aficionados. In the first, volunteers were encouraged to add one avocado to their daily menu for 12 weeks. Their weight and BMI didn’t change, nor did their blood sugar and insulin. But . . .
Women subjects (not men) were found to have significantly less visceral fat at the end of the avocado regimen. No, that didn’t mean they had flatter tummies. Disappointed?
Don’t be. Visceral adipose tissue (VAT) is a significant contributor to the risk of cardiometabolic disease. It’s not outside, it’s inside, and can’t be detected with a tape measure. Rather, it requires a scan to penetrate the body and calculate intra-abdominal fat stores.
I had it done once, and was pleased to find my score was less than one; A rating between 1 and 12 indicates that you have a healthy level of visceral fat. A rating between 13 and 59 indicates that you have an excessive level of visceral fat.
Then there’s additional good news on the nut front: A pecan-rich diet was shown to reduce cholesterol—particularly the “bad” LDL kind. Participants who ate 68 grams—that’s a lot of pecans (about 2 and 1/2 ounces)—for just 8 weeks enjoyed an average drop in cholesterol of 5% and between 6% and 9% in LDL.
Walnuts also scored big vs. heart risk in a recent study. Walnuts are rich in fiber, plant sterols, and omega-3-fatty acids. After two years of walnut consumption, participants lowered their cholesterol by 8.5%, and their LDL by 4.3%. There was also a beneficial reduction in small, dense LDL of 6.1%.
I make sure to sprinkle some crushed walnuts on my salads; walnut or pecan butters, while pricey, are other tasty ways to meet your nut quotient.
CAVEAT: These were all industry-sponsored studies. But then so too is much published research that shows efficacy of drugs.