Purpose:“Men on active surveillance (AS) for prostate cancer are extremely interested in dietary changes or supplements to prevent progression of their disease. We sought to determine whether a high omega-3, low omega-6 fatty acid diet with fish oil capsules (D + FO) decreases proliferation (Ki-67) in prostate biopsies in men with prostate cancer on AS over a 1-year time period.”
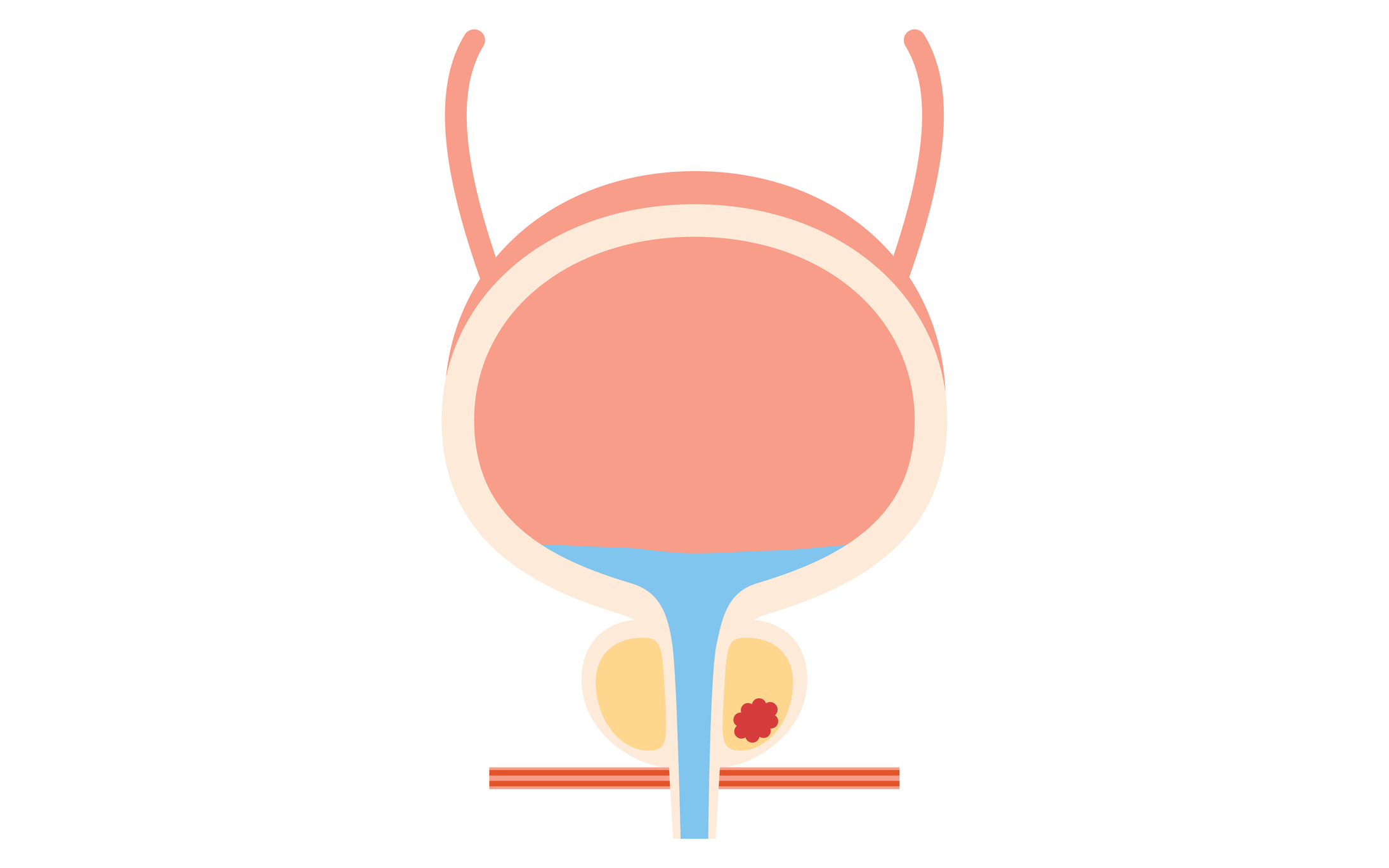
Methods: “In this phase II, prospective randomized trial, men (N = 100) with grade group 1 or 2 prostate cancer who elected AS were randomly assigned to the D + FO or a control group. Same-site prostate biopsies were obtained at baseline and 1 year. The primary end point was the change in Ki-67 index from baseline to 1 year from same-site biopsies compared between the groups.”
[The Ki-67 index is used to measure the aggressiveness of cancer based on analysis of biopsy specimens. The higher the index, the greater the likelihood a cancer will grow rapidly and metastasize]
Conclusion:“A high omega-3, low omega-6 diet with FO for 1 year resulted in a significant reduction in Ki-67 index, a biomarker for prostate cancer progression, metastasis, and death.”
COMMENT: Time was, if you had a diagnosis of prostate cancer, you’d be automatically relegated to the choice of either surgery or radiation treatment—with or without chemical “castration” to starve the cancer of testosterone. These treatments are associated with a high risk of side effects like urinary incontinence, erectile dysfunction, and general debilitation. Hormone therapy increases the risk of metabolic syndrome, a pathway to premature cardiovascular death.
This notwithstanding the recognition that a considerable percentage of men over the age of 70 harbor small, slow-growing foci of prostate cancer—the kind that the body’s natural cancer surveillance could keep in check for decades, long after a man might succumb to other age-related threats to longevity.
It was only in the 90s that studies confirmed the safety and practicality of “watchful waiting”, soon redubbed “active surveillance”. By means of better analysis of biopsy specimens for aggressiveness of tumors, and via deployment of sequential PSAs for monitoring, some patients could be selected for conservative treatment with active surveillance.
It’s counterintuitive for a doctor to proclaim: “You have cancer. Don’t just stand there, do nothing!” It took a while, but waiting has now become the preferred treatment for low-grade, localized prostate cancer. It can be a little nerve-wracking for patients, who have been conditioned to believe that once you have cancer, it should be rooted out. Especially men, who are action-oriented. Even our vocabulary needs to change; there’s our “War Against Cancer”, we “fight cancer”, and sometimes succumb after “a courageous battle against cancer”.
In the 90s, through the collaboration of Aaron Katz MD and Geo Espinoza ND, then at Columbia Physicians and Surgeons urology department, the concept was refined to “active holistic surveillance” under the premise that diet and lifestyle could influence outcomes, and reduce the likelihood that men undergoing monitoring would require medical or surgical interventions.
A 2016 study confirmed the feasibility of active holistic surveillance for delaying progression to advanced prostate cancer:
235 men with early-stage localized prostate cancer underwent extensive lifestyle counseling involving diet, exercise and stress reduction along with “chemopreventive” supplements. 88% of the men stuck with the regimen for one year and there were no prostate cancer deaths; 99.6% of them survived, which was remarkable for a group of men as old as 88, suggesting ancillary benefits of the program for allmajor causes of death.
Now comes the CAPFISH-3 Study, which seems to further validate the “holistic” component of active surveillance. The intervention chosen was to alter the Omega 3:6 ratio of dietary precursors by supplementing with fish oil, while reducing sources of Omega-6 fats.
There’s biological plausibility to the notion that omega-3s might prevent cancer via their anti-inflammatory benefits. They’re also said to be pro-apoptotic, meaning they can encourage “immortal” cancer cells to self-destruct.
A recent study confirmed the oft-asserted deleterious effect of elevated omega-6:3 ratios:
“Our findings extended to the inverse associations of plasma omega-6 and omega-3 PUFAs with 14 site-specific cancers.”
But the authors added:
“One notable exception to this trend of protective association was a positive association between omega-3 PUFAs and prostate cancer.”
By contrast, the CAPFISH-3 study confirms the benefits of altering the Omega 3:6 ratio in prostate cancer.
This imbalance is often asserted to be a feature of modern diets’ radical departure from their Paleolithic origins. According to a review, during our prehistoric past, that dietary ratio was around 1:1; now it’s more like 1:14 or 1:25, indicating a severe mismatch between our modern food environment and the genes we’ve inherited over thousands of years of natural selection.
So, the altered ratio may not be a cause of cancer per se, but rather simply indicative of an overall poor diet which predisposes to cancer.
While seed oils are currently in the crosshairs, it remains controversial whether Omega-6 fats, per se, are cancer-promoting, or if it’s their ubiquity in ultra-processed foods that makes their reduction beneficial. Sources of Omega-6 fats include fried and fast foods, baked goods, candy and confections, dressings and condiments, and meat and dairy substitutes.
It’s likely that other components of active holistic surveillance like weight optimization, exercise, adequate sleep, refined carbohydrate reduction, microbiome interventions, avoidance of xenoestrogens, and chemo-prevention via vitamins like D, and nutraceuticals like melatonin, curcumin, lycopene, green tea, etc. will be shown to contribute to the success of conservative management of low-grade prostate cancer.
Parenthetically, there’s a move afoot to apply a similar model of active surveillance to other small, or early, low-grade cancers like DCIS (ductal carcinoma in situ of the breast) in women. Traditionally treated aggressively, there are new calls for forbearance.
Modeled after prostate cancer, these developments might usher in an entirely new era of opportunities for integrative oncology with active holistic surveillance.
See also “Fish Oil and Prostate Cancer” by Karolyn Gazella