On a recent episode of Intelligent Medicine, I highlighted a study that demonstrated that an anti-inflammatory diet could halt or slow progression of 59 different chronic diseases. We’ve known for a long time that inflammation is a hallmark of “Inflammaging”, a precursor to frailty, and that a wide gamut of conditions—cardiovascular disease, autoimmunity, neurodegenerative diseases, musculoskeletal disorders, liver and kidney diseases, diabetes, and cancer, among them—are linked to inflammation.
But I took issue with one of the premises of the study: That red meat was included among foods designated “pro-inflammatory”.
The study relied on something called the DII—the dietary inflammatory index—to rate foods according to their potential to prevent or promote inflammation. First released in 2004, it’s said to be a work in progress as studies help to refine it.
An article in Harvard Health (“Foods that fight inflammation”) sums it up:
Foods that cause inflammation
Try to avoid or limit these foods as much as possible:
- refined carbohydrates, such as white bread and pastries
- French fries and other fried foods
- soda and other sugar-sweetened beverages
- red meat (burgers, steaks) and processed meat (hot dogs, sausage)
- margarine, shortening, and lard
On my broadcast, I maintained that the inclusion of red meat, and even lard, in that list of horribles was unsubstantiated. It’s reflective of bad science tainted by an anti-animal protein bias.
Could America’s definers of dietary rectitude be wrong?
I sought to dig deeper to find support for my contention that, when it comes to inflammation, red meat—or even saturated fat—are not the culprits.
Of course, you can do yourself in with too much red meat. Wasn’t that the point of “Supersize Me”, in which the late Morgan Spurlock gorged on Big Macs and was soon warned by his physician that he was on death’s door?
But that’s precisely the point: Any diet that features a surfeit of animal protein complemented by inordinately high levels of French fries, soda, and sugar laden milkshakes is going to be pro-inflammatory. An overabundance of calories, especially in the setting of a sedentary lifestyle, promotes obesity. And obesity per se is pro-inflammatory!
And that’s where the science gets mixed up. Large studies alleging the harms of meat consumption are often confounded by the mere fact that a fairly high percentage of meat eaters are like Morgan Spurlock—they’re indiscriminate eaters, in contradistinction to plant-centric eaters, who are more fastidious about their caloric intake and their lifestyles in general.
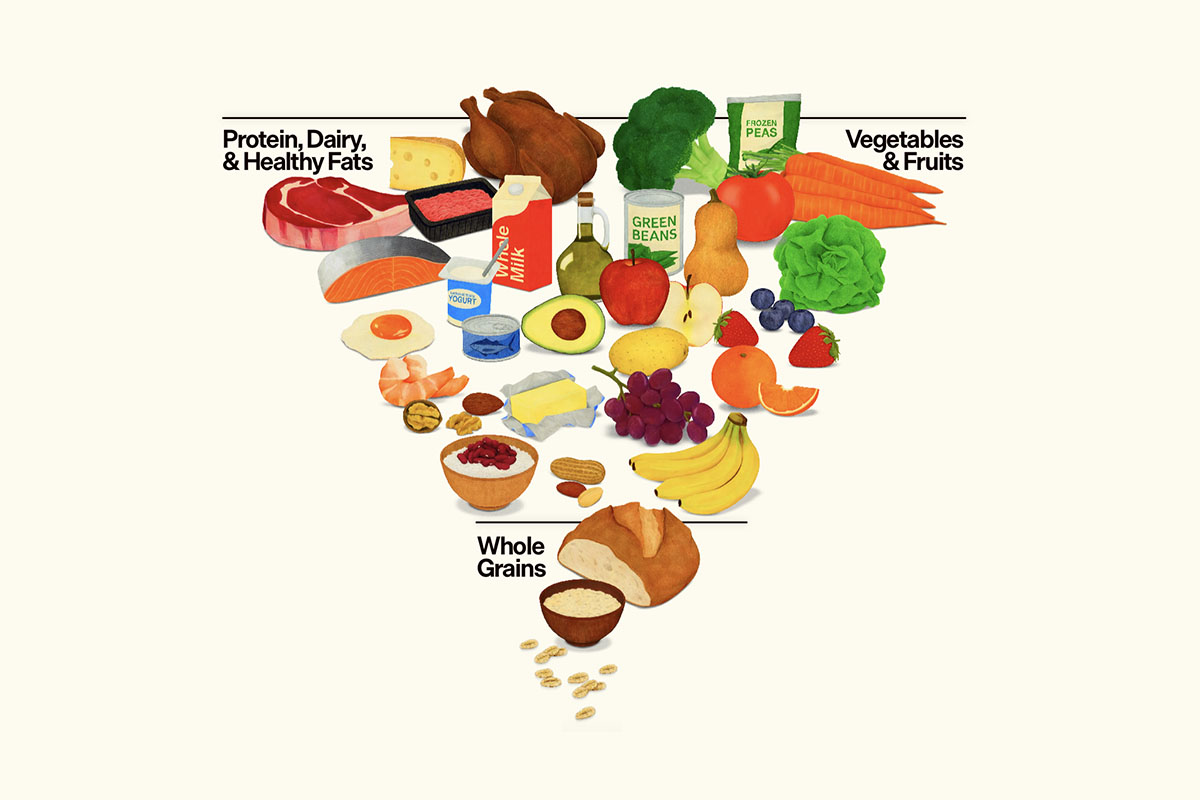
What about folks like me—and possibly you—who eat liberal amounts of meat (mostly organic or range-fed), but in the context of a diet rich in anti-inflammatory compounds from spices, tea, olive oil, nuts, fruits and vegetables, and bereft of sugar and high-glycemic ultra-processed junk?
Are there studies that exonerate red meat as a promoter of inflammation? I thought so, and it turns out there are.
In an article entitled “BMI, not red meat may directly contribute to inflammation”, Medical News Today heralds a study that points out:
“Previous speculation suggests that eating red meat leads to higher levels of inflammation and thus contributes to increased risk for cardiovascular disease. A recent study’s evidence, however, indicates that red meat consumption is not associated with inflammation, and instead, this link has more to do with body mass index.”
The study that MNT references states:
“In analyses that adjust for BMI, neither processed nor unprocessed forms of red meat were associated with any markers of inflammation . . . Our analyses were unable to support a relationship between either processed or unprocessed red meat and inflammation, over and above any confounding by BMI.”
Of particular interest was the absence of a link between red meat intake and C-reactive protein (CRP), the major inflammatory risk marker of chronic disease.
But surely, anti-meat crusaders will counter, it’s not so much that meat is bad, it’s the dangerous saturated fat it contains that stokes inflammation. Hence frequent admonitions to choose lean cuts of meat, to remove skin from chicken, and to favor low-fat dairy alternatives.
Does saturated fat promote inflammation? Many health authorities would have you believe so. But that dogma deserves reconsideration.
A study in adolescents sought to explore the possible link between saturated fat consumption and inflammation as measured by high-sensitivity C-reactive protein (hsCRP, commonly regarded as a potent cardiovascular risk factor). The researchers summarize:
“Saturated fatty acids (SFA) have been reported to promote inflammation. Nevertheless, evidence linking dietary SFA and low-grade inflammation in adolescents is scarce and inconsistent . . . Our findings do not support a detrimental role of dietary SFA in low-grade inflammation among adolescents. In males, higher dietary SFA was associated with lower hsCRP.”
Of note, the study authors found that higher levels of exercise made the association of saturated fat consumption with lower hsCRP even stronger. This suggests that exercise mitigates the caloric impact of saturated fat consumption among physically active meat consumers.
When it comes to full-fat dairy, there’s no indication that it increases propensity to inflammation. In fact studies have found the opposite. One review summarizes:
“The consumption of milk or dairy products did not show a pro-inflammatory effect in healthy subjects or individuals with metabolic abnormalities. The majority of studies documented a significant anti-inflammatory effect in both healthy and metabolically abnormal subjects.”
Meat, while generally thought to be rich in saturated fats like stearic and palmitic acids, varies in composition according to source. Grass-fed or pastured meats are generally lower in fat, and their composition favors more polyunsaturated Omega-3 fatty acids which deliver anti-inflammatory benefits.
But lard—surely that’s pro-inflammatory, isn’t it? Well . . . it depends.
Traditional lard, while much maligned, has been a staple of ancient diets, and varies in fat makeup according to what animals are fed (“You are what you eat eats!”). It actually averages only 39% saturated fat, the rest being beneficial monounsaturated and polyunsaturated fat—with a minimum of the Omega-6s we get too much of. Crisco and other modern industrially processed shortenings that make their way into most fried foods, baked goods, and confections, by contrast, are made up of mostly pro-inflammatory refined soybean oil and hydrogenated palm oil.
Natural—but not factory-made—lard is even a rich source of vitamin D; each tablespoon delivers 1000 I.U.s!
Many animal studies that purport to demonstrate the deleterious effects of saturated fat consumption utilize Crisco as rat chow!
The ultimate test case for the inflammatory impact of meat and saturated fat is the ketogenic diet, rich in animal protein, and supplying the majority of its energy from saturated fat, in lieu of carbohydrates. A recent review, “The effect of a ketogenic diet on inflammation-related markers: a systematic review and meta-analysis of randomized controlled trials”, addressed that question. The verdict:
“ . . . adherence to a KD appears to improve some markers associated with inflammation, including TNF-α and IL-6.”
The ketogenic diet quelled inflammation particularly well in at-risk subjects who were overweight or obese.
Finally, the Framingham Offspring Study, one of the world’s longest observational studies examining the relationship between diet and heart disease (begun in 1971), concluded this about the relationship between saturated fat consumption and heart disease:
“In this US community-based cohort of mainly Caucasian women and men, we found no evidence to support an adverse relationship between any type of dietary fat and several cardiometabolic risk factors, including lipids, adiposity, inflammation, and glucose.”
Moreover, dietary fat seemed to confer a slight protective effect:
“ . . . we also found that all types of dietary fat were associated with larger protective HDL particle sizes in both men and women. Women with higher intakes of all fat types also had higher concentrations of HDL particles, while for men, this was the case only in association with saturated and monounsaturated fats. Further, both saturated and monounsaturated fat consumption among men was associated with larger LDL particle sizes which are less atherogenic than the small dense particles that are more prone to oxidation.”
We can conclude that many previous studies implicating saturated fat as the cause of inflammation have proceeded from the premise that meat is bad, and have tortured the data to jibe with their predetermined conclusion.
All this distracts us from the real culprits: sugar and refined carbohydrates. In a study of premenopausal women with overweight and obesity, researchers concluded:
“Our findings illustrated that high-carbohydrate intake was associated with a high level of inflammatory state. While, fat intake did not have any statistically significant relationship with inflammatory markers.”
Hence, the purveyors of lists of anti-inflammatory foods evidently have some catching-up to do when it comes to red meat.