“Make sure you stay well hydrated!” As a health imperative, it seems a little lightweight—unless you happen to be a Tour de France contestant. It conjures up visions of legions of ultra-thin young women obsessively slugging back mountain water in plastic bottles like cowboys swilling whiskey in a Wild West saloon.
Too often doctors are dismissive of pop culture exhortations to pay attention to hydration. Except for those with specific medical conditions, the conventional mantra remains “In ordinary healthy individuals, thirst is a good guide to how much fluid you should consume.”
In medicine, we routinely query patients about their diets, their exercise, their sleep, their stress levels, drug, alcohol and tobacco use, their social interactions, their spirituality, even their sexuality. But so seldom do we ask “How’s your hydration?”
A recent review found that, “Hypohydration is known to reduce mental and physical performance, and more recent evidence suggests hypohydration also impairs vascular function and cardiovascular regulation.”
But adequate fluid intake is not merely a matter of optimization; a recent medical study sampling 1200 adults aged 51-70 suggests that it may literally be a matter of life and death:
“ . . . underhydration was significantly associated with increased prevalence of obesity, high waist circumference, insulin resistance, diabetes, low HDL, hypertension, and metabolic syndrome. Over 3–6 years of follow-up, 33 chronic disease deaths occurred in the sample, representing an estimated 1,084,144 deaths in the U.S. Alongside chronic health conditions, underhydration was a risk factor for an estimated 863,305 deaths. Independent of the chronic health conditions evaluated, underhydration was a risk factor for 128,107 deaths.”
How prevalent is underhydration in a sample of American adults? According to the study:
“Nationally representative data from the National Health and Nutrition Examination Survey (NHANES) indicate that over 65% of adults aged 51–70 years in the U.S. do not meet hydration criteria.”
What constituted underhydration? They didn’t just ask participants how much they drank, where recall is notoriously inaccurate. They relied on objective measures like high blood sodium, low volume of urine production, and high concentration of urine.
There’s no way to spot check your blood sodium at home (Apple Watch developers take heed), but a simple hack is to look at your urine color. Barring high intake of B vitamins, which can turn your pee magic marker yellow, the toilet water should resemble dilute lemonade.
There’s even evidence that differences in hydration may account for health disparities. It’s well known that socioeconomically disadvantaged populations have poorer medical outcomes—increased infant and maternal mortality, increased risk of heart disease, diabetes, hypertension and kidney failure, and curtailed longevity. We can blame poorer health literacy, bad diets fueled by “food deserts”—more recently supplanted with the term “food apartheid”, limited physical activity in unsafe neighborhoods that aren’t walk-friendly, stress of economic insecurity, inequitable access to quality medical care, even the psychological toll of racism itself.
But lately studies are singling out underhydration as a significant risk factor for vulnerable populations. A recent paper (“Cross-sectional analysis of racial differences in hydration and neighborhood deprivation in young adults”) concludes:
“Our data suggest that compared with White young adults, Black young adults are hypohydrated . . . and that greater neighborhood deprivation is associated with chronic underhydration irrespective of race.”
Why should this be the case? The authors speculate that concern over water quality leads economically-challenged persons to skimp on tap water, the cheapest and most readily-available source of fluid repletion. Indeed, recent revelations like that of lead contamination in Flint, Michigan and a CNN headline heralding the presence of “forever chemicals” in half of U.S. tap water, substantiate these fears.
Distrust of water supplies has an unforeseen dire consequence, according to a study entitled “The relationship of perceptions of tap water safety with intake of sugar-sweetened beverages and plain water among US adults”:
“Overall, 13.0% of participants disagreed that their local tap water was safe to drink and 26.4% of participants agreed that bottled water was safer than tap water . . . The associations of tap water mistrust with intake of SSB [sugar-sweetened beverage] and plain water were modified by race/ethnicity . . . Non-white racial/ethnic groups who disagreed that their local tap water was safe to drink were more likely to report low intake of plain water. The odds of consuming ≥1 SSB per day among Hispanics who mistrusted their local tap water was twice that of Hispanics who did not.”
Resorting to alcoholic beverages as a “safer” alternative to tap water is no better; they have a net dehydrating effect.
Disparities affect kids, too. A 2015 study asserted:
“Children’s hydration status could have implications for both health and school performance. Two studies have shown that inadequate hydration, defined as urine osmolality of 800 milliosmoles per kilogram or higher, is associated with poorer performance on cognitive tests . . . Inadequate hydration is a prevalent and understudied health problem among US children and adolescents, particularly boys, non-Hispanic Blacks, and Hispanics.”
And indeed they found:
“ . . . more than half of all children were inadequately hydrated. Younger children, boys, and non-Hispanic Blacks had higher urine osmolality than older children, girls, and non-Hispanic Whites. The odds of inadequate hydration were 1.76 times higher among boys than girls and 1.34 times higher among non-Hispanic Blacks than non-Hispanic Whites.”
So how much should you really drink? You’ve probably heard the advice to drink eight glasses of water per day. That’s an aspirational goal for most healthy people, but it lacks nuance and individualization. Thirst alone is not always a useful benchmark; for the elderly, and for those with certain medical conditions or taking some medications, the sensation of thirst may be blunted.
The U.S. National Academies of Science, Engineering and Medicine have suggested that an adequate daily fluid intake is:
- About 15.5 cups (3.7 liters) of fluids a day for men
- About 11.5 cups (2.7 liters) of fluids a day for women
If that sounds like a lot, keep in mind that these recommendations comprise fluids from water, other beverages and food. About 20% of daily fluid intake usually comes from food and the rest from drinks.
Most ultra-processed foods are desiccated—think chips, pretzels, cheesy snacks, cookies, and candies. Others, like processed meats, pizza, dressings, sauces and condiments, are high in sodium, which increases hydration demands.
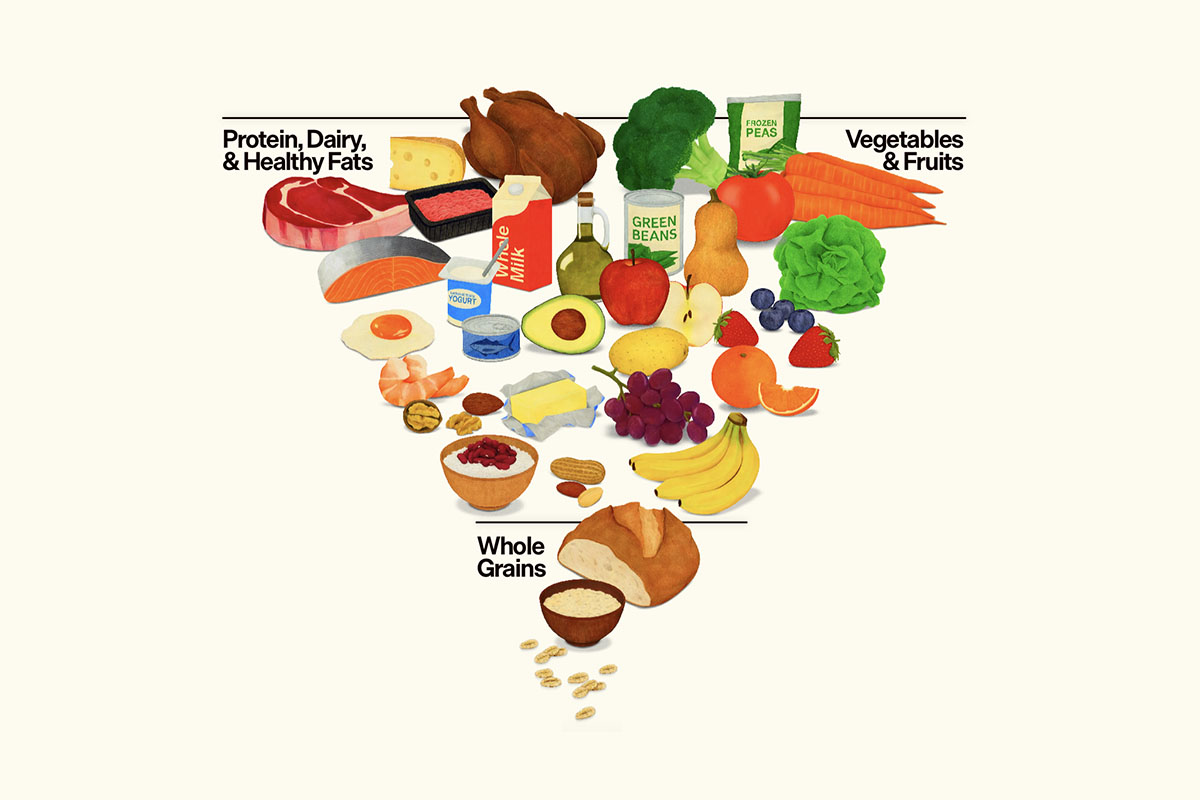
Fresh fruits, vegetables, legumes and whole grains are rich in fiber, which has the ability to create a fluid matrix. Hence the term soluble, fiber—which means “able to be dissolved, especially in water.” That means that, to some extent, you can “eat your water” via proper food selection.
Of course, there’s the danger of too much of a good thing—overhydration. It can cause fatigue, lightheadedness, muscle weakness, and if severe, brain swelling resulting in coma and death. It happens when people consume too much water, especially when unaccompanied by electrolytes. Ultradistance athletes who consume plain water must be especially cognizant of this, or they’ll end up in the medical tent. But I’ve seen healthy young women who engage in obsessive water consumption—compounded by rigorous salt avoidance—who feel weak, woozy, and “washed out”. Curtailing excess fluids and liberalizing sodium is restorative.
Paradoxically, the very demographic most vulnerable to the adverse effects of underhydration —the elderly—may scrimp on fluid intake. Prostate problems, decreased bladder capacity and urinary leakage discourage drinking. In fact, before side effect-laden drugs are invoked, first line treatment for urinary frequency and nocturia (nighttime awakening to void) is officially recommended to be behavioral; patients are encouraged to curtail excessive beverages before bedtime.
These recommendations need to be balanced with the imperative to maintain adequate hydration. Underhydration is a threat to well-being as well as an instigator of disease and avoidable death that can’t be minimized.