A recent TV ad for a new expensive osteoporosis drug, Evenity®, seeks to create the impression that women are fragile porcelain dolls, teetering on the brink of toppling and shattering.
Hype aside, osteoporosis is a thing. Three million fragility fractures of the hip and spine occur each year in the United States; osteoporotic fractures have been shown to account for loss of more Disability Adjusted Life Years (DALYs) than most common cancers. A hip fracture in a frail senior can be a death sentence with an almost a 30% one-year mortality rate. An estimated 30 million individuals in the U.S. suffer from osteoporosis.
A diagnosis of osteoporosis is not as cut-and-dried as, say, a positive HIV test. An arbitrary cutoff of a T-score of minus 2.5 means you’ve crossed the threshold from osteopenia—normal age-related bone loss—to osteoporosis. A “0” score means you have the bone density of an average healthy 30-year-old female (male rates are adjusted); each 1.0 point decline from zero means an additional 10-12% reduction from ideal. Minus 2.5 suggests you’re around 25% below a 30-year-old at peak bone mass. That might be a harbinger of fragility if you’re 50, with a lot of years ahead of you to lose bone, but it’s average if you’re 85. A low T-score merely heightens the odds for a fracture; it cannot predict with certainty you will or won’t have one.
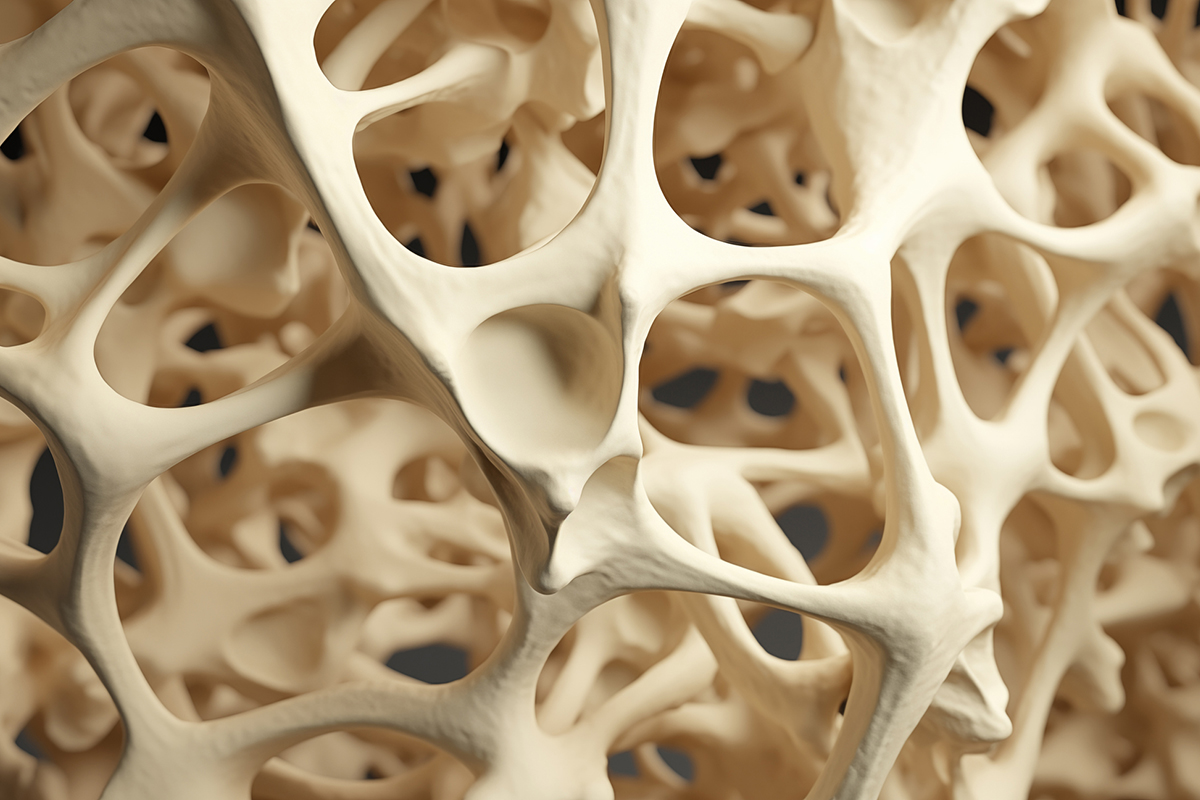
Our current way of assessing osteoporosis risk is crude and imprecise. It relies on the DEXA bone densitometry. It measures bone quantity, but not bone quality. Bone may appear dense, but it may be brittle, like a piece of chalk. Certain drugs, like fluoride, demonstrably increase bone density, but don’t prevent bones from breaking.
DEXAs are also static, like GPS positioning while you’re driving. To establish your time to destination, you need the speed at which your vehicle is traveling, or in the case of bone, the rate at which bone health is improving or deteriorating. Moreover, DEXAs change slowly, usually reflecting meaningful change at intervals of no less than two years. Hence, it’s hard to assess progression—sometimes until it’s too late—or alternatively, to gauge the effectiveness of interventions. A trajectory of several readings gathered over six or eight years is sometimes necessary to verify a trend.
Technicians I’ve talked to also report that proper positioning is crucial to accurately capture DEXA images; variation in operator technique or equipment calibration can produce “wobble” in results.
It’s fair to say that the most definitive fracture risk assessment would be to take an individual and drop them from progressively greater heights!
Short of that extreme measure, to correct the limitations of sole reliance on a DEXA score, osteoporosis authorities have developed the FRAX index. It’s a calculation of your 10-year risk of a fragility fracture based on your DEXA while factoring in family history of fracture, whether or not you’ve had a previous break, smoking, alcohol use, steroid medication, exercise, age, sex and weight (here’s where carrying a few extra pounds may be beneficial!) You can test-drive the FRAX calculator here.
While a refinement of the DEXA alone, the FRAX index is still an imperfect tool. What are needed are better methods to assess bone quality and resilience, and also the rate at which bone loss (or gain) is occurring.
For the latter we already have some promising tools that measure byproducts of collagen degradation—so-called bone turnover markers (BTMs). They can be measured in blood or urine.
There are two basic types of BTMs: Bone resorption and bone formation markers. They can be used to assess the rate of bone turnover, which is reflective of the rate of progression of bone loss. They go by an alphabet soup of names like NTX, PINP, and beta-CTX. They can also be used to assess the effectiveness of therapy, as when lifestyle or medication demonstrates slowing of the shedding of collagen degradation byproducts in the blood or urine. But the optimal ranges for these markers are not as ironclad as the T-scores derived from DEXA—guidelines for their interpretation are still being worked out. Research is also underway to monitor the messenger RNA molecules that reflect bone regeneration as indices of bone health.
When it comes to visualizing bone quality, a variety of promising technologies are vying to outperform the DEXA. A proper analogy is to the ultrasound for assessing the risk of liver disease; regular scans can quantitate liver fat, but only spot fibrosis when it’s advanced; the new Fibroscan®️ (liver elastography) actually determines whether the liver is losing flexibility as fibrotic tissue replaces healthy liver cells.
The trabecular bone score (TBS) looks at textural changes within the DEXA which reflect the microarchitecture of bone. It’s been validated in studies and has been shown to enhance the predictive accuracy of the DEXA. And it’s available at various centers in the U.S. although insurance coverage is variable.
Then there’s quantitative CT (QCT) which uses low-dose radiation to create a precise 3D picture of bone. Limitations include higher cost as well as cumulative exposure to ionized radiation with serial exams.
Radiofrequency echographic multi spectrometry (REMS) is an innovative approach that uses ultrasound to analyze bone mineral density. REMS can provide an estimation of bone strength (fragility index) which is independent from a DEXA T-score and has been shown to effectively predict fracture risk. REMS hasn’t caught on for use in the U.S. but it’s received endorsements from European osteoporosis authorities.
Regardless of whether these are superior technologies, they face obstacles due to medical economics, regulatory barriers, and sheer institutional inertia. There’s also the fear of medical liability whenever tried and true modalities, however inferior, are supplanted by novel screening methods. And rationing—euphemistically dubbed “cost-containment”—often keeps us from the best care. That’s why adoption often trails innovation by decades.
All this is predicated on the reductive notion that fracture risk is merely a reflection of the degree of osteoporosis. Lower extremity muscle strength, balance, vision, and cognition are strong determinants, as I point out in a previous article “Keep your balance”. Two women with identical T-scores may be at dramatically divergent risks of a fragility fracture depending on their susceptibility to falls.
Japanese researchers have developed a prediction model for falls among older people. Using data from questionnaires and physical assessment, they claim “an individual’s risk of falls over the course of a year could be predicted with acceptable sensitivity and specificity.”
Finally, work is underway to identify robust genetic predictors of osteoporosis. Genes that determine receptivity to vitamin D, collagen durability, and susceptibility to inflammation are likely candidates. A one-off saliva test can reveal hereditary vulnerabilities.
All this can be TMI for the brain of even the most astute clinician to crunch. But the promise is that machine learning, trained on large data sets of correlations between test results and outcomes, can reveal consistent patterns. Artificial intelligence, and the ubiquity of fast processors, may help doctors develop a “Super-FRAX” algorithm way more predictive than sole reliance on old-school DEXAs. Data using questionnaires, genetic profiling, physical exam and strength and balance assessment, blood and urine tests, and sophisticated imaging can be collated into a more precise predictor.
We need to bring more nuance to decisions on whether to use powerful meds to forestall osteoporosis. Too many women are indiscriminately placed on drugs when they don’t really need them; others are left unprotected while at high risk for fractures. Moreover, we need better tools to assess the efficacy of lifestyle measures and pharmaceutical interventions. They can even help us decide when a “drug holiday” makes sense after years of treatment.
That’s where the future of fracture prediction may lie . . . if we have the wisdom and resources to commit to it.