



| By Dr. Ronald Hoffman
Isabel, a choreographer in her mid-40s, came into my office and said, “I don’t know if something is happening to me. I can’t remember the name of this step when I’m teaching; I use it all the time, but I start to say it in class and it just doesn’t come. And yesterday in class I kept saying ‘left’ when I meant ‘right.’ Is something happening to my brain?” Well, Isabel was just tired and stressed that week, and the following week she had no trouble with names or directions in any of her classes. But many of us wonder sometimes, when we can’t recall a name that is totally familiar to us, whether something is wrong with us. These worries take on a little more weight as we grow older, because we do know that there’s some degree of memory loss with aging. Many have had the disturbing experience of talking to an aged, ill person who seems to have forgotten big chunks of what happened that morning or even the names or faces of family members.
There is definitely a natural decline in short-term memory and learning ability with age, and it seems to be a slow, progressive decline. It has even earned a medical acronym: ARMI, for age-related memory impairment. There also are physiological changes in the nervous system with age—some of the neurons in the brain die off. On the other hand, studies suggest that older people may actually be able to improve in some areas of intelligence and mental ability, such as the ability to verbalize complex ideas and global comprehension—the ability to synthesize meaning from a lot of data. Another word for this might be wisdom.
Human intelligence may adapt naturally to the accumulation of memories and experience. As data accumulate, the brain learns to make leaps or bridges to find the common ground, the means of integrating experience, so that we aren’t simply submerged in the endless details of life. So maybe it’s a mistake to talk about a decline in memory and intelligence with age, when what really happens is a qualitative change. It may be more difficult to go to law school or medical school and memorize a lot of minutiae at the age of 50 than at the age of 20. On the other hand, it’s no accident that world leaders and business executives in their 50s and 60s and 70s are able to make major decisions about complex issues and balance huge agendas every day. Clearly, they’re not suffering from mental decline. And many artists from Pablo Picasso to Martha Graham to Henri Matisse have seemed to lose little of their creativity with age. Though neurons can deteriorate as the brain ages, intelligence and alertness can be compatible with very advanced age.
In fact, recent studies have shown that a global decline in mental function with age is not at all inevitable. About 25 percent of people in their 80s who volunteer for cognitive testing perform just as well as volunteers in their 30s and 40s. So the moral is, for the brain as for the rest of the body, use it or lose it!
There also are nutritional aspects to brain function in older people. Vitamin B12 plays an especially important role. Many cases of Alzheimer’s disease and senile dementia share a component of undiagnosed or borderline deficiency of vitamin B12—a kind of selective malnutrition. I have given vitamin B12 supplements, or even injections, to some elderly patients and seen a sharp increase in general alertness and mental responsiveness.
Beyond stimulation and nutrition, there are unfortunately some pathological processes that affect memory. The two major ones are cerebrovascular disease and Alzheimer’s disease, and many people are afflicted with several degenerative processes. Cerebrovascular disease, which affects the circulation of blood in the brain, can cause a progressive decline in memory. At the same time, someone who has changes in personality, memory and understanding at an advanced age may be suffering from the degenerative features of both cerebrovascular disease and Alzheimer’s. We do know quite a bit about cerebrovascular disease and how to prevent it, so let’s look at that first.
Starving the brain: Cerebrovascular disease
The brain requires 20 percent of the body’s oxygen and is extremely sensitive to a deficient blood supply. In fact, there is some speculation that most age-related senility may be linked to decreased blood flow in the brain rather than to degeneration of the tissues and nerves. Some striking research to support this has been done with a natural extract from leaves of the ginkgo biloba tree, which increases blood flow in the brain and actually improves memory and attention in elderly patients as well as short-term memory in younger volunteers. Maintaining a healthy supply of blood to the brain is essential to normal mental function and may help prevent what we think of as age-related memory loss.
When blood flow to the brain is sharply reduced, usually through gradual degeneration of the blood vessels, some form of cerebrovascular disease is present. In fact, this is really an atherosclerosis of the brain, with hardening and narrowing of arteries caused by the buildup of fatty cholesterol deposits. The result of severe cerebrovascular disease often is a major blood-supply failure: a stroke. There are two types of strokes: those caused by a blood clot in narrowed arteries, which cuts off blood to portions of the brain, and those caused by rupture of a blood vessel and the hemorrhaging of blood into brain tissue, often called apoplexy or cerebral hemorrhage. Both kinds of stroke can “black out” major portions of the brain, such as speech centers and movement centers. They can cause partial paralysis, partial blindness, dizziness, slurred speech, mental confusion and personality changes. The symptoms may strike immediately or worsen more slowly over hours or days. Sometimes persistent long-term therapy can lead to complete or partial recovery, but often the damage is permanent.
Not everyone who suffers from cerebrovascular disease will have a stroke, but many will have TIAs — transient ischemic attacks — which are short, passing ministrokes caused by temporary constriction of blood flow. They can cause temporary blackouts, dizziness, numbness or slurring of speech. Real damage may be done, but not in such a dramatic way that you’d think to rush someone to a hospital. Many others will not experience even these symptoms, but with progressive reduction in blood flow to the brain will suffer a decline in thinking ability, balance, memory, emotional stability, sleep patterns or any other functions regulated by the brain.
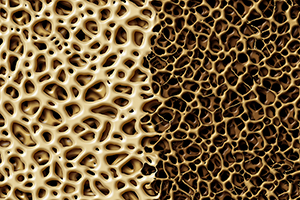
If we use sophisticated CAT scans or MRI to look at the brain of someone suffering from cerebrovascular disease, we may see little gaps or holes—a “Swiss cheese” look that neurologists call an etat lacunaire (literally, the “condition of lacunae”). What we see are all the tiny portions of the brain that have simply died because of impaired circulation or ministrokes. The holes or lacunae represent dead tissue, and this kind of damage certainly affects brain function.
The good news is that the ongoing degenerative process of cerebrovascular disease can be prevented and possibly even arrested once it’s begun. Let’s look at some of the risk factors.
Risk factors for cerebrovascular disease
The effects of cerebrovascular disease usually don’t show up until advanced age, but the stage is set much earlier. The risk factors are primarily the same as those for heart disease: a high-fat diet, smoking, poorly controlled blood pressure and insufficient nutrients, especially antioxidants. In fact, we are now seeing cerebrovascular disease symptoms in younger people in their 40s and 50s who smoke, are alcoholic or have hypertension. It’s interesting that the incidence of heart disease in Japan is very low because of a low-fat diet. But the incidence of strokes there is quite high, because the Japanese diet has a high level of salt, which causes high blood pressure and strokes. An,d frankly, cerebrovascular disease also is a disease of poverty. Many socioeconomically disadvantaged groups suffer from poor medical care and poor treatment for hypertension, eat poor-quality fast food or processed food that’s laden with sodium or fat, and are more susceptible to alcohol and smoking problems because of life pressures and stresses. They can wind up on a fast track to cerebrovascular disease.
High blood pressure has been shown to lead to mental decline and may accelerate the pace of cerebrovascular disease. Studies have shown that people with chronic high blood pressure, especially over a period of years, have the greatest decline in mental tasks that involve short-term memory. In fact, the studies show a direct correlation between specific, measured rates of increase of blood pressure and scores on memory tests. There is some evidence that high blood pressure may reduce the oxygen supply to the brain and increase tissue damage in the tiny arteries of the brain.
Alcohol consumption only is a moderate risk factor for heart disease and can even have a protective effect at low levels. However, it seriously increases the risk of strokes and cerebrovascular disease, even at fairly low levels. Anything more than two drinks daily for men and two or three weekly for women, is associated with higher risk of stroke.
Diagnosing cerebrovascular disease: Conventional treatment
Since the damage from cerebrovascular disease builds up very slowly, the damage has already been done by the time someone has symptoms or a recognizable pattern on a CAT scan. However, some new tests can offer an early warning. The Doppler test does an ultrasound scan of the carotid artery, the biggest blood vessel that supplies the brain. If it shows signs of constriction, and the fatty deposits and hardening of artery walls we call atherosclerosis, it’s a fair bet that there’s pervasive atherosclerosis throughout the cerebral vascular system. A newer technology called MRA, magnetic resonance angiography, will enable us to visualize the soft tissue of the arteries and the flow characteristics of blood. This can directly reveal atherosclerosis in cerebral blood vessels.
As with cardiovascular disease, current treatments attempt to bypass portions of the diseased carotid artery or use the balloon angioplasty technique to loosen and expand a hardened artery. These are fairly risky procedures and sometimes can cause a stroke themselves. In fact, the guidelines for performing this type of surgery were recently made more stringent because the potential benefits were thought to not justify the risk. Worse, “fixing” the carotid artery does not help hardened and clogged arteries within the brain itself.
As for medication, there’s some evidence that taking an aspirin a day can help prevent stroke as well as heart disease. A whole new generation of drugs, of the calcium channel blocker family, selectively dilate blood vessels in the brain but are not very satisfactory on the whole. Then there are various blood thinners, but they can be problematic; anything that thins the blood and therefore promotes bleeding may cause hemorrhagic or “bleeding” stroke.
Since none of the high-tech approaches for treating stroke or cerebrovascular disease are very safe or effective, this is one more case where we’re led straight back to prevention as the best “treatment.” Fortunately, this disease process can be prevented or arrested in most individuals if they start early enough. And the best way to start is by following the protocol for preventing heart disease, including a low-fat, low-sugar, low-sodium diet; regular exercise; avoidance of smoking and excess alcohol intake; and sufficient heart-healthy nutrients.
Nutritional supplements: A key support system
Here’s a master list summarizing the supplements that are key in preventing heart disease.
Vitamin C is helpful in preventing arteriosclerosis.
Recommended: 1,000 milligrams daily.
Mixed carotenoids are excellent antioxidants shown to reduce the likelihood of arteriosclerosis.
Recommended: 25,000 international units daily.
Vitamin E is extremely helpful for reducing the stickiness of platelets and improving blood flow. It also tends to slow the progression of arteriosclerosis and may have something to do with reversing it.
Recommended: 400 to 800 international units daily.
EPA fish oil oil is a natural blood thinner.
Recommended: two or three 1,000-milligram capsules twice daily.
L-carnitine is a natural agent for helping to promote energy production in the cardiac muscle cells.
Recommended: one 500- to 1,000-milligram capsule twice daily.
Co-enzyme Q10 is another catalyst for energy production in the cardiac muscles.
Recommended: 100 to 400 milligrams daily.
Calcium, with magnesium, helps control blood pressure.
Recommended: 400 milligrams daily.
Magnesium plays a role in preventing arterial spasm.
Recommended: 400 to 800 milligrams in chelated form daily; or magnesium citrate, 200 milligrams twice daily.
Though we think of declining estrogen as the hallmark of menopause, it's actually common for…

Up to 12 percent of Americans have ulcers at some point in life. Peptic ulcers…
Gallbladder disease is a modern illness. An estimated 20 million Americans have gallbladder disease. The…

Lately, I’ve been sharing with Intelligent Medicine listeners that I’ve been augmenting my diet with…
Q: I am a 77-year-old woman. On recent bone density test, lumbar spine results range…

The 1973 sci-fi movie Soylent Green depicts a dystopian future in which over-population and environmental…

A New Era in Wellness: Non-CBD Innovations with Lex Pelger, Part 1

Our virtual voicemail is open 24/7, so there's no need to wait to submit your questions for Dr. Hoffman. Leave a message, and you may hear your question featured on the Intelligent Medicine radio program!