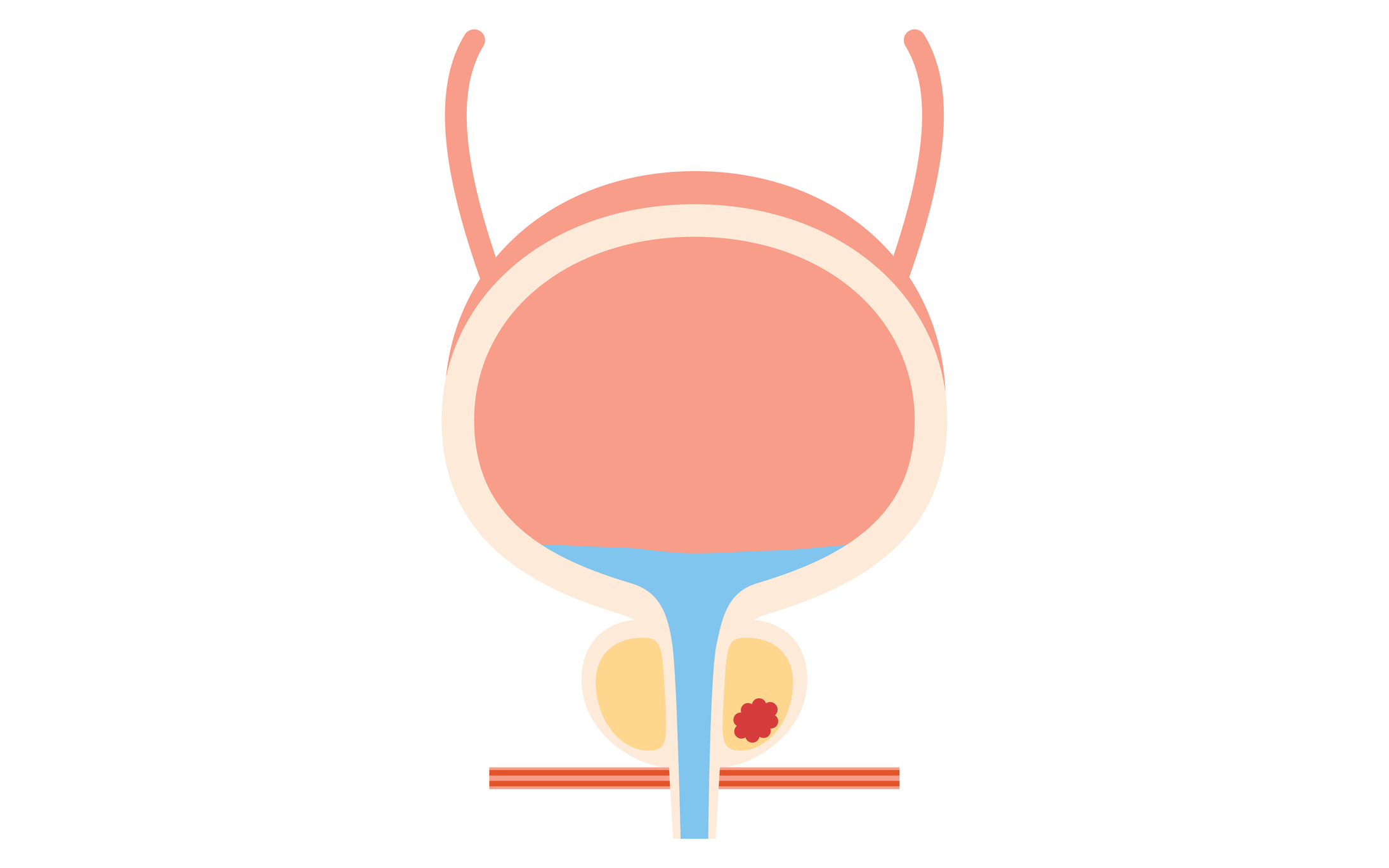
Sooner or later, most American men will have a rendezvous with the prostate gland. This doesn’t have to mean prostate cancer, but two very common prostate problems can cause quite a bit of discomfort. The first, prostatitis, is an infection or inflammation that can affect men of any age. The second, benign prostatic hypertrophy, is a fancy name for the enlargement of the prostate gland that affects many men in their 60s and 70s. The main side effect is that the enlarged gland squeezes the urethra, making it difficult to empty the bladder and causing frequent, dissatisfying urination.
What is the prostate? It’s a small gland about the size of a walnut that encircles the urethra and is mostly a factory for spermatic fluid. The prostate gland gives us the name for prostaglandins, which are chemical messengers that affect everything from inflammation to blood pressure. Embryologically, the origin of the prostate is similar to the origin of the uterus, and both of those organs affect the metabolism of prostaglandins. The prostate gland produces lots of prostaglandins, but they also are produced in every tissue of the body. The prostate does not have a profound effect on general metabolism, though it may have an effect that is not currently understood or appreciated. Men who have the prostate removed don’t have a significant change in their overall bodily prostaglandin levels. Unfortunately, the presence of all those prostaglandins in this small organ make the prostate gland reactive and finicky so that an inflammation process that starts there can get out of hand.
Prostatitis: Who can you talk to?
This leads us to a very common but little understood and little discussed “men’s problem”: prostatitis. This is a catchall term for an inflammation of the prostate gland, which can cause a painful, burning sensation during urination and, in fact, can produce a fairly steady experience of pain in the groin. Men who have prostatitis in their late 20s or 30s often are struck with a sense that they’re entering a degenerative phase. They recollect their father or grandfather experiencing prostate trouble—”plumbing problems,” as they used to be called—but there’s little connection at all between prostatitis and the prostate enlargement so common in older men.
What’s unfortunate is that prostatitis afflicts men in unprecedented numbers, but most men experience it in isolation. While women very commonly and very easily share stories about their breasts, reproductive organs, infections and symptoms, most men just don’t talk about their bodies. It’s difficult for many men to get beyond ordinary conversation to a discussion of their prostate, even with a close friend. They can be in agony and not talking to anyone and not getting much relief from the urologist. (This is changing with the recent establishment of a National Institutes of Health task force on prostatitis.)
Prostatitis may be one of the legacies of the sexual revolution. It often seems to start with a mild sexually transmitted infection, whether viral or bacterial, that makes its way into the highly sequestered prostate gland and sets off a cascade of inflammatory reactions that can persist for months or even years, long after the infection should have worn itself out. There aren’t many blood vessels in the prostate, so it can be harder to get medications such as antibiotics in there through the blood stream. It’s not even clear that an infection is necessary to keep the inflammation going. Sometimes a urologist can isolate a bacterium from the prostatic fluid, sometimes not. Sometimes the inflammation will flare up with a change in sexual habits, such as a period of heavy sexual activity after long abstinence.
Urologists try different antibiotics, but they don’t always work. One of my patients, James, told me of his own nightmare experience. He’d contracted a sexually transmitted disease after a one-night stand, and he was having the typical burning urination and was pretty much in pain all the time. He went to his internist, who prescribed a course of tetracycline. That didn’t seem to help, so he saw a urologist, who prescribed a different antibiotic. That didn’t help, either. Over the next two years, he ended up seeing about ten different urologists, who prescribed more antibiotics, different antibiotics, sulfa drugs, beta blockers to “relax” him, Valium and even Librium, which gave him crying jags. None of them were able to isolate or identify an infectious agent, and some would go on and on about how “clear and normal” his urine looked. Several suggested that he should see a psychiatrist, but he was in daily, constant pain.
To add insult to injury, he had to keep bending over to submit to the standard manual exam of the prostate at each office visit. To perform the standard examination, a doctor puts on rubber gloves, daubs two fingers with Vaseline, and inserts them up the anus to manually palpate the prostate gland in order to check for pain or enlargement and sometimes to cause emission of some spermatic fluid for testing. James told me he’d had about enough of this for a lifetime.
Finally, in despair, he wrote a letter to one of the top urologists in the country, at a major New York teaching hospital, to ask whether there was anything that could be done. This doctor had the courtesy and refreshing honesty to write back saying, “Unfortunately, medical science doesn’t really know all that much about what causes this problem or keeps it going, and we don’t have any surefire remedy for it. We know it’s painful and upsetting, but fortunately, it often does seem to die out of its own accord.”
My patient was so relieved to have this specialist “come clean,” as it were, that he stopped hunting down new urologists and new medications, and resigned himself to waiting it out. Sure enough, the pain did slowly lessen over the course of another year, and a few years later it was just a memory.
That said, there are some steps you can take to alleviate the situation. There are more sophisticated tests now, and it’s worth trying to get a bit of the spermatic fluid to culture for bacteria. Some urologists will advise the patient to increase sexual activity on the theory that it is better to relieve pressure and release the prostatic fluid that may be harboring an infectious agent. Another doctor might dolorously advise reducing sexual activity if someone is relatively active. Sometimes these maneuvers help. Alcohol and caffeine seem to increase the burning sensation, so they should be avoided. Physical stress, sitting for prolonged periods and, especially, lack of sleep seem to make the inflammation worse, so simply slowing down a bit may help. Warm sitz baths sometimes provide relief.
For prostatitis, I prescribe Prostat, a flower pollen extract, which has been shown in European and Japanese studies to have a positive effect on the inflammation. I think it’s important to consider this not just as an infection but as an inflammatory disease. A chronic inflammatory process still can be churning away, even in the absence of any virus or bacteria. Prostatitis can sometimes be allergic, and a food allergy profile may be worth doing. If the prostate is already inflamed, and thereby predisposed, it could react to an allergen in the diet.
Because the prostate is a rich source of prostaglandins, some of which play a part in the inflammatory process, inflammation is a special problem for this organ. The different types of prostaglandins mediate in a sort of yin-and-yang way in the body. The “bad prostaglandins” constrict blood vessels and bronchial tubes, produce inflammation and may exacerbate symptoms of PMS in women. The “good prostaglandins” reduce inflammation, and cause blood vessels and bronchial tubes to dilate. Accordingly, an imbalance in prostaglandin metabolism could easily set the stage for chronic inflammation of the prostate. I don’t think anti-inflammatory medication is a good long-term solution because in order to reduce inflammation it inhibits all prostaglandins—the good ones as well as the bad ones. If we could find a way to selectively inhibit the bad prostaglandins without inhibiting the good ones, we’d have a good therapy for prostatitis. (“Good” and “bad” are relative terms, of course, because inflammation and constriction of blood vessels are to some extent a useful response to a wound or an infection.)
One way to restore prostaglandin imbalance is to provide the precursors of the “good” prostaglandins, which are the essential fatty acids (EFAs), i.e., alpha-linolenic acid and linoleic acid. These are present in good ratios in flaxseed oil, which may therefore support the prostate in making the “good prostaglandins,” the ones that reduce inflammation. The “bad prostaglandins” are derived from arachidonic acid, which is present in meat, so a diet high in meat and dairy products may contribute to prostate disease. Gamma-linoleic acid (GLA), found in primrose, black currant and borage oil, also may help soothe the inflamed prostate.
In the future, I think we may find that some of the “bugs” that inhabit the prostate, if they’re there at all, may be what’s called “cell-wall-deficient organisms.” They are very difficult to culture and difficult to eradicate, because most antibiotics kill bacteria by attacking the cell wall. Medical science may one day advance to the point of identifying and targeting them. But for now, any man who is struggling with prostatitis should console himself with the knowledge that this problem usually does die away with time.
The aging prostate
Most American men will need to face two issues as they head into their 50s, 60s and 70s. They are prostate enlargement and prostate cancer, which are sometimes, but not necessarily, related. It is very common to have prostate enlargement without cancer. In fact, prostate enlargement is virtually universal among North American men, while prostate cancer is not. Nevertheless, it’s estimated that the vast majority of men may have “microfoci” of cancer: tiny clusters of cancer cells that are normally of very little consequence because they are slow-growing. But some of them can develop down the line.
Prostate enlargement, or benign prostatic hypertrophy (BPH), is that annoying development that many men associate with their older fathers: the frequent urination pattern that would send them to the bathroom several times during dinner or get them up repeatedly during the night. The enlargement that squeezes the urethra can kick in as early as the late 40s, though it’s more common in the 50s, 60s and 70s.
While common in the United States, BPH is much less prevalent in some other parts of the world, so environment, lifestyle and diet clearly play a large part in it. Both prostate enlargement and prostate cancer are much less frequent in Japan, for example, apparently because of the higher consumption of soy, beans and the cabbage family, all of which contain phytoestrogens (or isoflavones), which are cancer-inhibiting. Researchers have found much higher levels of these phytoestrogens in the blood of Japanese men than in Occidental men. They appear to have a blocking effect against prostate cancer and prostate disease in general.
Diet also affects prostaglandin metabolism, which may be important for prostate health. The arachidonic acid present in meats stimulates production of the “bad prostaglandins,” while the American diet is generally deficient in the essential fatty acids—the omega-3 oils and the omega-6 oils—that promote the “good prostaglandins.” The omega-3 oils are found in cold-water fish such as tuna, salmon, herring, trout, mackerel, sardines and cod liver, as well as nuts, including walnuts, and seeds, including pumpkin, which also are high in prostate-protective zinc. Omega-6 oils are found in vegetable sources, including primrose oil, borage oil and black currant seed oil.
A common surgical treatment for enlarged prostate is the transurethral resection of the prostate (TURP), which employs a kind of plumber’s snake that goes up the urethra and shaves off part of the gland without removing it totally. New studies have suggested that this procedure should not be as casually employed as it once was because it leaves a significant percentage of men with impotence or flow problems and even, rarely, leads to death.
Newer treatments including laser, microwave and freezing are in the wings, but prudence dictates that surgery not be used at the first sign of symptoms but rather saved as a last resort. A promising new therapy, transurethral needle ablation (TUNA), uses radio waves to zap prostate tissue, obviating side effects such as incontinence, impotence or retrograde ejaculation. One heavily marketed prostate-shrinking medication, Proscar, works by blocking a hormone that can cause the prostate to enlarge. (The hormone is DHT, dihydrotestosterone, a major cause of prostate growth.) But Proscar doesn’t work for everyone, and although the prostate may shrink, the urinary symptoms may not abate. Some men have seen an improvement in their urinary symptoms over two weeks to four months, but there can be serious side effects, including lowered libido or impotence, breast swelling or allergic reactions. Prostate-specific antigen levels are altered, possibly masking the development of prostate cancer during treatment. Even more seriously, prostatic fluid transmitted sexually to a woman who becomes pregnant may cause genital abnormality in a male fetus. Some men achieve better results with blood pressure medications such as Hytrin or Cardura, but these may cause side effects, such as dizziness.
An alternative natural therapy is extract of saw palmetto. This can take a little longer to work, but it avoids the side effects of drugs. One study found that 160 milligrams twice daily of standardized extract of saw palmetto (Serenoa repens) caused an improvement in quality-of-life scores, urinary flow rates and prostate size after a month and a half. Another natural therapy uses extracts of the bark of Pygeum africanum, a tropical African evergreen tree, in a dosage of 50 to 100 milligrams twice daily. Several studies have reported on its positive effects.
Prostate cancer
We have a new perspective on prostate cancer in the 1990s, which is both promising and troubling. The development of the prostate-specific antigen (PSA) test has vastly increased our ability to detect cancer in the prostate long before it would become evident through manual examination or malignant enlargement. It should stand to reason that better detection would result in a vast improvement of statistics on prostate cancer, but it hasn’t, and this has been quite distressing. Though our detection skills have increased, we unfortunately have not made any real advances in treatment.
The standard treatments—radiation or complete removal of the prostate—are not always effective because a few cancerous cells can remain in surrounding tissue and spread to other parts of the body, usually the bones. On the other hand, in men older than 70, the vast majority of prostate cancers are relatively indolent. Someone with incipient prostate cancer may have a somewhat diminished life expectancy, but it could be as long as 12 to 15 years, over which time most men of this age succumb to other causes of death. Surgery and radiation at this age may not ultimately slow the progress of cancer and may have other harmful side effects, which can themselves increase the chance of death. Accordingly, “W.W.”—watchful waiting—is increasingly indicated. In fact, this approach is being used in such a variety of ailments that it’s becoming one of the most popular “therapies” of the 1990s. If “W.W.” were a drug, I’d say buy stock in it.
The PSA test quickly is becoming part of a standard blood workup that men get with their annual health exam. Its increasing sophistication, coupled with the lack of improved therapies, has generated a bitter controversy among medical scientists and clinicians. They ask whether the test is telling us more than we need to know. Some say, “How can you deny anyone this information about a potentially life-threatening disease?” Others respond, “What good does it do, since it won’t change medical management and may just induce anxiety to no useful purpose.” I think that the information should be made available and that it’s worth having an annual PSA test after the age of 50 or when symptoms warrant in a man younger than 50. But the information should be used with appropriate restrain by men who are aware that watchful waiting is a good option. Men younger than 70 whose PSA test result is positive might be advised to consider more aggressive treatment options.