I recently interviewed Dr. Erika Schwartz, a leading women’s healthcare specialist, and author of The New Hormone Solution. I was surprised at her answer when I asked about osteoporosis drugs:
“Of all the medical options available, which do you prefer?”
“None of them,” she answered
“None of them?”
“That’s right. I believe hormone replacement therapy, properly administered to women at the time of menopause, along with weight-bearing exercise, are the most effective ways to forestall bone loss. The osteoporosis drugs carry risks that outweigh their benefits and don’t need to be used if we start bio-identical hormones at menopause and women remain active.”
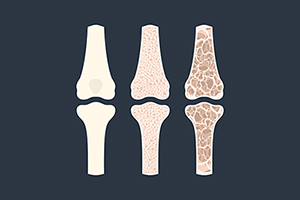
I used to be an osteoporosis screening “hawk”; I fell in line with the conventional wisdom that sussing out premature bone loss with a DEXA bone densitometry was a must for women hitting menopause, when bone loss begins to accelerate.
And yet, a recent position paper from the U.S. Preventive Services Task Force (USPSTF) is causing me to re-examine my beliefs. More on that later.
No doubt BigPharma and the medical device industry have done a great sell job with their “osteoporosis awareness” campaigns. Last year, I wrote:
“A recent TV ad for a new expensive osteoporosis drug, Evenity®, seeks to create the impression that women are fragile porcelain dolls, teetering on the brink of toppling and shattering.”
Pharmaceutical companies are responsible for 39% of the annual revenues of the advocacy group, the Bone Health and Osteoporosis Foundation; other contributors include manufacturers of screening equipment like Hologic (maker of DEXA). The stated goal of BHOF is to “End fractures caused by osteoporosis”.
According to Cognitive Market Research, the global market for one popular category of osteoporosis drugs—bisphosphonates like Fosamax, Actonel and Boniva was 4.125 billion dollars in 2024 and will expand at a compound annual growth rate (CAGR) of 4.30% from 2024 to 2031. North America holds the major market of more than 40% of the global revenue with a market size of USD 1.65 billion dollars in 2024 and will grow at a compound annual growth rate (CAGR) of 2.5% from 2024 to 2031.
In 2022, the global market for Prolia, a newer, pricier osteoporosis drug, was valued at $2.9 billion dollars. By 2030, the global Prolia market is expected to reach $7.2 billion dollars. The retail price of Prolia, without insurance reimbursement or rebates, is $1,875.43 per injection, which must be administered every six months, sometimes indefinitely. Most patients don’t pay the full price due to insurance coverage and/or patient assistance programs. Some patients are hit with enormous co-pays, as well as charges for an IV infusion, which must be administered under medical supervision.
Screening is lucrative, too. An ad directed at doctors and clinics entitled “How A DEXA Scan Machine Boosts Revenue For Your Business” boasts: “You got into the medical, health, or fitness industry with the hopes of changing lives for the better. A DEXA scan machine can help you not only improve the health of your patients but can boost your revenue and grow your practice. The global DEXA market is expected to reach $1.2 billion by 2024. This growth is driven primarily by the health issues that will organically rise as the geriatric population grows. By 2030, seniors are predicted to outnumber children for the first time in U.S. history.”
The market for DEXA is projected to grow at a rate of 8% annually to reach a total of 1.57 billion dollars by 2029.
But the latest USPSTF position paper is hardly a ringing endorsement of aggressive screening and treatment.
Entitled “Screening for Osteoporosis to Prevent Fractures: A Systematic Evidence Review for the US Preventive Services Task Force” (published Feb. 11, 2025) it concluded that benefits of screening were seen only in high-risk women [older than] 65. The benefits of screening younger women at time of menopause, as reflected in a number-needed-to-treat analysis, were small:
“Corresponding absolute risk differences were 5 to 6 fewer fractures per 1000 participants screened.”
They added that, even with addition of a commonly used algorithm, the FRAX index, predictive value was poor:
“Risk assessment instruments, BMD alone, FRAX, or both have poor to modest discrimination for predicting fracture.”
They summarized: “Given these uncertainties, before ordering BMD tests in younger postmenopausal women, clinicians should counsel patients about the lack of evidence regarding benefits vs harms of initiating osteoporosis drug treatment at this life stage.”
When it came to screening men—at any age—the evidence was even more scant:
“The USPSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of screening for osteoporosis to prevent osteoporotic fractures in men.”
They also did not recommend forearm testing for risk assessment.
A June 2024 review in the American Journal of Medicine expresses the uncertainty about screening to inform the decision to start drugs:
“Prevention of osteoporotic fractures is an important health concern and worthy of careful consideration in shared decision-making by clinicians and patients. Risk assessment including history of fractures should guide decision making. For patients at high risk of fracture, especially those with prior fractures, treatment with bisphosphonates is well supported by clinical evidence that may underestimate benefits; however, for patients with osteoporosis based on bone density alone, treatment benefits are less certain. Hip fracture risk reduction is modest and not supported in patients without a history of fracture. Reductions in vertebral fractures are substantial regardless of baseline risk, but whether these reductions correspond to less chronic pain and disability is unclear. Clinical evidence is weaker for newer agents. Future guidelines and reviews on osteoporosis treatment should clearly distinguish between primary and secondary prevention of fractures to best inform clinical decision-making. Despite guideline recommendations and calls for more screening and treatment, there are legitimate reasons for some clinicians and patients to opt out.”
Benefits of bisphosphonates are real, but since they interfere with bone remodeling, continuous long term use (more than five years) may lead to brittle bone and paradoxically increase the risk of atypical fragility fractures; osteonecrosis of the jaw is an infrequent but serious side effect of prolonged use.
An overlooked downside of Fosamax, the oldest and most frequently prescribed bisphosphonate, is its potential effect on mood. A Naturereview states:
“The use of alendronate [Fosamax] and other bisphosphonates has been associated with depressive symptoms in recent case reports . . . The reported risk of depressive ADRs [adverse drug reactions] was found to be over 14-fold greater in patients taking alendronate under the age of 65 and over fourfold greater for patients over 65 compared to the control.”
Newly-popular Prolia has been shown to reverse osteoporosis but its absolute risk reduction is modest: A mere 0.4% decrease in hip fractures.
And when a course of Prolia therapy is discontinued, there is “rebound” acceleration of bone loss, necessitating initiation of a bisphosphonate drug for an indefinite period.
Since Prolia is a biological medicine that acts on the immune system, Drugs.com cautions:
“Research has shown people who take Prolia are at an increased risk of serious infections leading to hospitalizations, including serious infections of the skin, abdominal, urinary tract, and ear. There is also a higher chance of developing endocarditis (an infection of the heart’s/ inner lining, usually involving the heart valves) in those who take Prolia . . . and for people administered concomitant immunosuppressant agents (such as prednisone or cyclosporine) or with impaired immune systems may be at an even higher risk. Doctors may need to consider discontinuing Prolia in people who develop serious infections or other severe side effects.”
Take-homes:
- Too many women (and men) are being unnecessarily placed on osteoporosis medication
- The benefits of medication have been oversold, and their drawbacks downplayed
- Screening for osteoporosis with DEXA bone densitometry (BMD) may be unnecessary for most healthy women under 65 and men of any age and lead to overzealous prescribing of medications
- We need better ways of determining who should and who shouldn’t be prescribed medications; BMD via DEXA scans should be augmented, or eventually supplanted, with superior predictors of fracture risk (see my article “We need better tests for osteoporosis”)
- More emphasis should be placed on optimizing bone health via diet, exercise, certain supplements, and bio-identical hormone replacement therapy initiated early in life, to forestall osteoporosis before it occurs
- The long-term risks/benefits of administration of osteoporosis drugs over extended periods (>5 years) need to be more throughly investigated; until then, it may be prudent to limit their duration of administration and to institute periodic “drug holidays” to enable normal bone remodeling to recover
- Fall prevention via balance training and lower extremity strength exercises should take precedence over pharmaceutical “fixes”