As you can see by this article that I wrote in 2013, I’ve long been concerned over side effects of commonly prescribed osteoporosis drugs. Among other worries, I raised a red flag over then newly-published reports of unusual fractures among women taking bisphosphonates, which include Fosamax, Actonel, Boniva and Reclast.
The bisphosphonates segment held the highest market size of around $445.74 million in 2017. Bisphosphonates are the most commonly prescribed medication for treatment and prevention of osteoporosis.
My suspicions were confirmed by research released in 2015 which documented the incidence of what are referred to as “atypical femoral fractures” (AFFs) in long-term users of these drugs. The average duration of treatment in women who suffered these fractures, sometimes at the slightest instigation like stepping off a curb, or with minor deceleration while strap-hanging in a subway, was seven years.
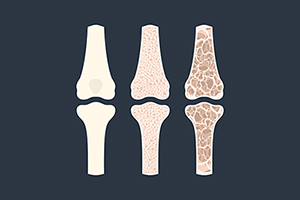
Researchers attribute this to a known mechanism of action of bisphosphonates: they increase bone density, but at the expense of impairing bone remodeling, which is essential for bone strength.
There’s circular reasoning applied to our approach to osteoporosis which fuels a multi-billion dollar industry. Routine screening tests that measure bone density (DXA scans) are a faulty proxy for the risk of eventual hip or spinal fracture; they become a gateway to prescribing drugs that women take for years, even decades. Subsequent improvements in the DXA score then provide (often false) reassurances that fracture risk is being mitigated.
A 2016 study found that 50.3% of women who received a prescription for osteoporosis medications merely had mild age-related bone loss (osteopenia). In women aged 40-64, inappropriate overtreatment with osteoporosis drugs was 66.4%.
Part of the problem is that the DXA—the “gold standard” for osteoporosis diagnosis and monitoring—relies on a crude metric: bone density. According to authors of a review article, that’s not enough to accurately predict fracture risk: “New imaging techniques that not only measure BMD but also measure critical indices directly related to fracture risk such as bone size, porosity, cortical thickness, trabecular volume and the mineral to matrix ratio are needed.”
I’ve long forecasted that someday we’ll come to think of the DXA as misleading and archaic. A bone biopsy might prove the ultimate reflection of skeletal health, but obviously non-invasive methods to assess bone quality are what we need. Several are being investigated in research settings, but aren’t ready for approval and commercialization.
But a newly-available test offers an enhancement over the conventional DXA—the Trabecular Bone Score (TBS). It’s not meant to supplant the DXA, but merely to enhance its predictive value. And cost won’t be much of a barrier to its widespread adoption. Clinics won’t have to invest in new multi-million dollar scanners. TBS is a software program that can be retrofitted to existing DXA devices, licensed to radiology clinics by GE Healthcare. They’re few and far between so far, but it’s likely many clinics will eventually adopt TBS. As of this year, it’s even reimbursed by insurances and Medicare.
For example, a woman might obtain a DXA T-score of minus 2.6 in her lumbar spine, which signals osteoporosis and heightened fracture risk. But a simultaneous TBS assessment might rate her bone quality as good, lessening the urgency of treatment. Alternatively, a program of supplements, diet and exercise might yield only trivial improvements in the DXA T-score, while substantially augmenting bone quality on the TBS, thereby incentivizing non-pharmacological interventions.
It’s early in the learning curve for TBS, and without further studies it’s unclear how insights about bone quality might shape clinical decision-making. Will it demonstrate that years-long use of osteoporosis drugs enhance or impair bone quality? Will some women be spared unnecessary medication via the feedback offered by TBS? Or will doctors continue to reflexively prescribe drugs to avoid potential liability, slow to trust a new modality?
Last month, it was revealed that we have even more reason to be wary of the most common class of osteoporosis drugs. Nature just published a study entitled, “Common osteoporosis drug associated with increased rates of depression and anxiety”.
The researchers compared rates of anxiety and depression among users of common bisphosphonate drugs. Incredibly, they found that users of Fosamax had a 14-fold greater likelihood of anxiety or depression if under 65; for users over 65 it was four-fold greater.
Other bisphosphonates were less likely to be associated with anxiety or depression, with Boniva and Actonel users with around doubled risk; Users of Reclast, an intravenous medication, were only 30% more likely to suffer anxiety or depression.
Now, the astute Intelligent Medicine reader might immediately recall my oft-repeated exhortation “correlation is not causation.” Maybe users of osteoporosis medication are more nervous to begin with, and more likely to seek out testing which yields the conclusion that they need medication. Or is it that high levels of stress elevate cortisol which boosts risk for bone loss? OK, but a 14-fold increase?
In addition, any good study has a control group. For this study, the control group was women who took a non-bisphosphonate medication—Prolia. They actually experienced a reduced incidence of anxiety and depression compared to the general populace. That suggests something real is going on with bisphosphonates.
For an association to be acknowledged as causal, it must be biologically plausible. That is, there must be a reasonable explanation based on known physiological mechanisms that accounts for the effect. Bisphosphonates are bone drugs; how could they possibly affect the brain?
The answer lies in the well-known principle of pharmacology that stipulates, for any given drug, there are off-target or pleiotropic effects. These can be beneficial or harmful. Hence the huge litany of side effects listed on package inserts for virtually all medications.
What the authors of this blockbuster article bring to the table are some enlightened guesses as to how Fosamax and its ilk might affect mood. I don’t want to go too deeply into the weeds on the complex biochemistry that underlies this, but they remind us that these drugs cross the blood-brain barrier, persist in the body for years, reduce calcium, affect acetylcholine (a key brain neurotransmitter), and impact certain neuron receptors linked to major depression.
All of which vindicates foregoing use of these medications unless absolutely necessary; it’s a rational choice. There are natural strategies which, in my decades-long experience, have equivalent benefits, without the drawbacks. But, as usual, you should consult your doctor to find out if these are appropriate for you—sometimes drugs will be needed to forestall the risk of debilitating fractures.