



Attention Deficit/Hyperactivity Disorder is a condition whose principal characteristics are inattention, hyperactivity and impulsivity. ADHD usually is diagnosed in children where the primary symptoms are difficulty controlling behavior and/or paying attention. According to the National Institutes of Health (NIH), it is estimated that approximately two million children in the United States have ADHD. This means in a classroom of 25 to 30 children, one will likely have ADHD. It affects all races and cultures, and boys are three times more likely to be diagnosed than girls.
How do we know it’s ADHD?
Not everyone who is impulsive, hyperactive or inattentive has ADHD. Actually, ADHD is not easy to diagnose, especially when inattentiveness such as daydreaming is the primary symptom. It is when a child’s distractibility, hyperactivity, poor concentration or impulsivity affects performance in school, behavior at home or in social relationships with other children that ADHD may be suspected. The diagnosis of ADHD requires that such behavior be demonstrated to a degree that is inappropriate for the individual’s age.
Approximately 20 to 30 percent of children with ADHD have a learning disability. In preschool years, these disabilities may present as difficulty understanding words or sounds and/or difficulty in self-expression. As children grow up, this can manifest as spelling or reading disabilities, and writing or arithmetic disorders.
Research estimates that between 30 and 70 percent of children with ADHD continue to exhibit symptoms in adulthood. For many, symptoms of ADHD do not become apparent until adulthood. Typically adults are unaware that they even have the disorder. They just feel that it’s almost impossible to get organized, keep an appointment or stick to a job. Distractibility, restlessness and impulsivity often are the characteristic symptoms in adults. Some may have a history of school failures, problems at work or been involved in frequent car accidents.
Scientists are now moving toward looking for a physiological basis for ADHD. Lately, an area of attention is the brain, particularly the frontal lobes of the cerebrum. This area of the brain allows us to restrain our impulses, solve problems and plan ahead. The left and right frontal lobes communicate with each other through the corpus callosum (nerve fibers). The basal ganglia are the interconnected gray masses in the cerebral hemisphere that connect the cerebrum and the cerebellum, which together are responsible for motor coordination. These parts of the brain have been studied through various imaging methods including the functional magnetic resonance imaging (fMRI), positron emission tomography (PET-scan) and single photon emission computed tomography (SPECT). A study conducted in 2002 of 152 boys and girls with ADHD showed a 3 to 4 percent smaller brain volume in all regions: the frontal lobes, cerebellum and temporal gray matter. (It is important to note that these imaging techniques remain research tools and cannot be used to diagnose ADHD in individuals.)
Catecholamines/neurotransmitters
Speaking of the brain, one area of focus in Intelligent Medicine is on deficiencies of the all important catecholamines. The catecholamines are dopamine, norepinephrine and epinephrine (commonly known as adrenaline). These “cats,” so cleverly termed by author Julia Ross, M.A., also function as neurotransmitters. Catecholamines arouse and excite us mentally, emotionally and physically, and help us to focus and be attentive. They keep us alert to the important events taking place around and within us so we can act quickly and decisively. These “cats” are said to be sleeping in an individual with ADHD. Low calorie, high carb diets cause catecholamine depletion due to inadequate protein intake. Our brains need amino acids from high protein foods such as eggs and salmon. Additionally, protein rich animal foods are high in the crucial amino acid tyrosine. For example, there are about 900 milligrams of tyrosine in a chicken breast, 840 milligrams in three scrambled eggs and 400 milligrams in a 4 ounce hamburger, but you would have to eat 24 almonds to get a scant 150 milligrams of tyrosine. Unfortunately, vegetable protein cannot compete. Vegetarians run the risk of catecholamine deficiency because of the typical low-protein nature of the diet. In fact, soy, a mainstay of a vegetarian diet, tends to inhibit the conversion of tyrosine into the catecholamines. Depletion of other micronutrients such as the B vitamins, calcium, magnesium and vitamins C and D also contribute to the problem. They are critical to adequate catecholamine function.
Perplexingly, some kids and adults with ADHD show features of both catecholamine insufficiency as well as catecholamine surges, made worse by hypoglycemia. This leads to a state of imbalance in the involuntary nervous system—something we call dysautonomia.
External and internal toxins
Environmental toxins from heavy metals such as lead, mercury and cadmium are certainly not to be overlooked in investigating and treating the causes of ADHD. Leaky gut from dysbiosis can initiate food allergies (most commonly to cow’s milk, wheat, corn, yeast, soy and eggs) as well as inhalant allergies—often a significant factor in many children diagnosed with ADHD. The noted allergist Dr. Doris J. Rapp points out a fascinating group of physical characteristics common among children with allergies, including red cheeks, red ears or ear lobes; dark or red circles or wrinkles under the eyes; and a horizontal crease in the nose that develops from what she calls the “allergic salute,” when a child with a runny nose rubs his nose upward with the heel of his hand.
The usual suspect initiators of leaky gut syndrome that usually precede food allergies are gluten and/or candida. Candida overgrowth often is the “master control” for food allergies, as well as a source of neuroactive endotoxins, which can make kids feel “stoned.” Other neurotoxins are MSG, aspartame (NutraSweet), and food colorings and additives. These can perpetuate ADHD symptoms to such peaks as to deem an individual behaviorally abnormal. Children appear to be particularly susceptible as their little bodies may be overwhelmed by “normal” doses of these toxins that are packaged in such innocuous substances as breakfast cereal and juice boxes. Detoxifying diets such as The Feingold Diet, which removes artificial flavors, colors, preservatives and salicylates, often bring about a significant decrease in symptoms, if not total abatement. Improved behavior can be observed in as little as one to six weeks (www.feingold.org). Helpful supplements to optimize nutrition status, initiate detoxification and address the deficiencies associated with ADHD are essential fatty acids (EFAs) such as Coromega or Orthomega (importance of this is discussed below), magnesium, calcium, probiotics, olive leaf, PectaSol, L-Glutamine, B complex, vitamin C, theanine, phosphatidylcholine, phosphatidylserine, zinc, B6 and its metabolite P5P (pyridoxal 5 phosphate).
Essential fatty acids are of critical importance in growth and brain metabolism. EFAs are present in cold-water fish and fish oils and in some vegetable sources such as flaxseed oil, borage and evening primrose oils. Studies have indicated that some children with ADHD have an altered fatty acid metabolism. EFAs, particularly DHA, is critical in brain development and IQ. Deficiencies of EFAs are associated with allergies, asthma, dry skin and hair, eczema, growth retardation and delayed puberty. Children on frequent antibiotic treatment for recurrent ear infections may develop EFA deficiencies. Supplementation as described above is beneficial.
The sugar/hypoglycemia connection
Pizza, bread, rice, french fries, spaghetti, sugared high-carbohydrate breakfast cereals and juice drinks are common dietary staples among young children. Not to mention the usual sweet treats children enjoy. Many children survive the sugar onslaught without discernable behavioral issues, but a smaller percentage of these children may be susceptible to behavioral reactions including powerful mood swings and physiological sensations as a result of their (and their parent’s!) chosen fuel. The oversecretion of insulin in response to eating these foods causes hypoglycemia, which then sets off the adrenals to secrete epinephrine in an effort to restore blood sugar levels. This is a major hormonal wallop for kids, causing them to go bouncing off the walls on a hypoglycemic roller-coaster ride.
The short list of symptoms of hypoglycemia includes weakness, fatigue, spaciness and an inability to concentrate. In adults, this hormonal cascade can cause symptoms ranging from short attention span to a full-blown panic attack.
For children and adults, restabilization of blood sugar is mandatory and includes tossing the refined “junk” carbohydrate food and drinks (a great opportunity to make a donation to your local food bank) and incorporating high-quality protein and fat at every meal. For the very symptomatic, five to six smaller meals every two to three hours throughout the day is therapeutic. I have patients who undergo personality changes if they don’t strictly adhere to this regimen. Supplements to complement a therapeutic diet in achieving stable blood sugar levels are chromium, L-Glutamine, GPLC, 5-HTP, tyrosine (to wipe out stubborn cravings), B complex and WellBetX PGX.
Current mainstream medical management of ADHD includes the use of stimulants such as Adderall, Ritalin, Concerta, Dexedrine, Focalin, Cylert and Metadate. Stimulants primarily work on the neurotransmitter dopamine. A recent addition to the list that is not a stimulant is Strattera. This medication works on norepinephrine. What these drugs do is physiologically push the individual into the normal range of behavior by rendering the individual more able to focus on one activity at a time. What these medications do not do is address the underlying problems that may be causing the abnormal behavior. It is important to remember that many of these drugs have side effects such as reduced appetite (not good for a growing child!), headaches and trouble falling asleep. It is worth noting that the NIH recommends that Cylert not be considered a first-line drug therapy because of its potential serious side effects affecting the liver.
Given the options offered by both complementary and mainstream medicine, there is much to be said for “first do no harm” where natural therapies are undertaken prior to falling back on more powerful but side effect-causing medications. True successful outcomes with symptom resolution can be brought about by first uncovering the underlying cause(s) of ADHD in the individual patient and then implementing the least harmful, most beneficial treatment.
References:
1. National Institutes of Health/National Institute of Mental Health (On-line). Attention Deficit Hyperactivity Disorder (2003). Accessed May 5, 2006.
2. Ross, J. The Mood Cure. New York, NY: Penguin Putnam; 2002.
3. Boris M, Mandel FS. Foods and additives are common causes of the attention deficit hyperactive disorder in children. Annals of Allergy. 1994;72:462-8.
4. Hoffman, RL. The Natural Approach to Attention Deficit Disorder (ADD). Los Angeles, CA: Keats Publishing; 1997.
Leyla Muedin is a clinical nutritionist and lecturer at the Hoffman Center and is available for speaking engagements for private and public sector wellness programs. Please call (212) 779-1744 for more information.
Though we think of declining estrogen as the hallmark of menopause, it's actually common for…

Up to 12 percent of Americans have ulcers at some point in life. Peptic ulcers…
Gallbladder disease is a modern illness. An estimated 20 million Americans have gallbladder disease. The…

Lately, I’ve been sharing with Intelligent Medicine listeners that I’ve been augmenting my diet with…
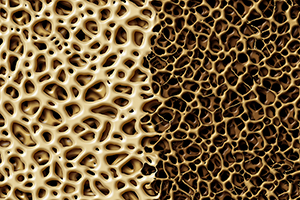
Q: I am a 77-year-old woman. On recent bone density test, lumbar spine results range…

The 1973 sci-fi movie Soylent Green depicts a dystopian future in which over-population and environmental…

Q&A with Leyla, Part 1: Copper Supplements

Our virtual voicemail is open 24/7, so there's no need to wait to submit your questions for Dr. Hoffman. Leave a message, and you may hear your question featured on the Intelligent Medicine radio program!