



| By Dr. Ronald Hoffman
What can you get from an injury, from a tick bite, from sex, from the food you eat, from lead poisoning or from a bacterial infection of the gut? Arthritis. What is it exactly? Well, the term is used pretty loosely to describe any kind of pain or dysfunction in a joint. It can be caused by dozens of factors that we know about and probably by others we’re still unaware of. In fact, it remains one of the less explored territories in modern medical science and may be just the common degenerative pathway for a whole array of different medical problems. It’s been with us for millennia—researchers have seen evidence of arthritic degeneration in the bones of Paleolithic men and women.
It can start with pain and stiffness in the neck when you get up in the morning, or a sore knee that you notice when you’re climbing stairs, or a gradually creaky shoulder that doesn’t seem to move freely, or soreness in the finger joints. Yet, you may not have suffered any injury; you don’t have a slipped disk; you didn’t do anything to stress the joint unduly. Well, you might be joining the ranks of the 49 million Americans who currently suffer from arthritis. That’s nearly one in four Americans—making arthritis one of the most common health conditions in the United States. In a few years you’ll probably have even more company—it’s estimated that by the year 2030 some 71 million people in the United States will have doctor-diagnosed arthritis. The estimated total cost associated with arthritis, including medical care and lost productivity, exceeds $86 billion according to the latest statistics from the Centers for Disease Control and Prevention.
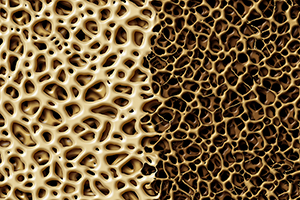
In most cases of arthritis, there’s inflammation and swelling of one or more joints; a simultaneous thinning of long, supportive bone shafts; and proliferation of extra bone material in the form of little spurs or protuberances in the joint itself. The bone spurs and the disease process start to damage the cartilage that cushions the two bone surfaces in a joint. As a result, the cartilage wears away and bone starts to grind against bone, causing pain, stiff joints and loss of range of motion. While cartilage and other tissue in the joints have normally few blood vessels, the arthritic disease process starts to infuse the area unnaturally with blood vessels, which carry in white blood cells, which in turn release immune factors called cytokines into the surrounding tissue, causing chronic inflammation.
This is the most common variety of arthritis, called osteoarthritis. It generally affects older people, though it can come on in midlife, especially after strain or trauma to the joints. This is the kind that affects an older person struggling to walk with painful hip or knee joints, or someone who is unable to hold a pen for writing or twist open a jar lid. Rheumatoid arthritis (RA), in distinction to osteoarthritis, can strike young and middle-aged individuals, especially women. In this condition, the joints become swollen, hot and tender, including joints of the feet, shoulders, elbows, wrists, hips, neck and lower back. Fatigue and anemia can accompany severe RA. It is primarily a disease of immune dysregulation, a kind of autoimmune disease, as if the body is attacking its own joints. (Though the factors are different, there is an immune component to osteoarthritis as well, since it’s an aberrant immune reaction that causes the inflammation to spiral out of control.) We don’t really know what causes rheumatoid arthritis, but there is mounting scientific evidence that suggests it is linked to vitamin D deficiency. It’s more common in industrialized countries, so there may be something about our Western diet or physical environment that increases the risk. The latest scientific evidence suggests consumption of more than three cups of coffee daily, particularly decaffeinated coffee, also may contribute. Tea consumption, however, is associated with decreased risk. I personally suspect that the man-made trans fatty acids or hydrogenated fats found in margarine and other foods may play a significant role in immune dysregulation by becoming incorporated into cell walls and interfering with the exquisitely delicate cell-to-cell communication that the immune system relies on.
We can diagnose osteoarthritis by looking at X-rays and seeing bone spurs, or at MRIs and seeing subtle changes in cartilage and joint fluid. We diagnose RA with sensitive blood tests that pick up levels of circulating proteins, called rheumatoid factors, that are associated with the disease. As in any medical syndrome, there are classic examples of each type and then individuals who seem to have a blending of symptoms and diagnostic factors. The disease doesn’t always match the paradigm. Classic rheumatoid arthritis is distinctive and is shown by the blood test, but then there are some puzzling cases of seronegative arthritis and palindromic arthritis that mimic RA but aren’t detected by the blood test.
What causes arthritis?
A better question might be, what doesn’t? Ten to one, if you ask why you have arthritis, your doctor will say, “Well, you’re not as young as you used to be. These things can happen when you get to be your age.” We simply don’t know what causes most cases of arthritis. At the same time, we do know of a long list of factors that can cause the disease in some individuals. They include trauma or injury, being overweight, genetic and environmental factors, allergic reactions and even some infectious diseases. Let’s look at some of these more closely.
Even this brief list of causative factors, still laced with unknowns, is enough to suggest that we should not simply accept arthritis as a common or even inevitable aspect of aging. Much research remains to be done, but even with this much to go on, we have begun to identify alternative treatments, which can improve on the relatively ineffective conventional treatments for both osteoarthritis and rheumatoid arthritis.
Treating arthritis: the conventional and natural approaches
Nowhere in medicine do we see sharper distinctions between conventional and alternative therapies than in the case of arthritis, especially RA. Comparing the way orthodox and nutritionally oriented physicians treat these conditions underscores the difference in philosophy between these two medical approaches. The high prevalence of poor outcomes and undesirable side effects in patients receiving conventional therapy and the beneficial results obtained by patients using alternative therapies suggests that the latter should be given greater attention than they are getting.
Even by the admission of many arthritis experts, conventional therapy for arthritis, especially for RA, is far less than optimal. The first step often is palliative therapy with aspirin or other non-steroidal anti-inflammatory drugs (NSAIDs) such as Motrin, Naprosyn, Voltaren, Clinoril, Ansaid, Relafen and, most recently, Celebrex, and the now-withdrawn Vioxx and Bextra. These drugs quench pain and stop inflammation to a certain extent, but they have little if any beneficial effect on the ultimate clinical course of arthritis. Some studies show that they may actually hasten joint damage. Many of these drugs possess several other unfortunate side effects, especially the tendency to cause stomach irritation, severe gastrointestinal bleeding and heart problems.
Steroid injections for arthritis and bursitis are another favorite tool of orthopedists. As we’ve noted, they are progressively less effective, and repeated injections can damage joints; oral prednisone can induce osteoporosis, cataracts, Cushingoid symptoms, elevated blood sugar, depression and even psychosis.
In the case of RA, doctors often prescribe more powerful second-line drugs. These are the so-called DMARDs (disease-modifying anti-rheumatic drugs). These agents are designed not just to control symptoms but actually to delay progression of the disease. Unfortunately, many of them can cause severe adverse effects. They include such drugs as hydroxychloroquine, sulfasalazine, prednisone, azathioprine, leflunomide, anakinra, tumor necrosis factor (TNF) antagonists such as infliximab and etanercept and methotrexate. The latter is a powerful chemotherapy drug used in the treatment of cancer. Some of these drugs possess potent immunosuppressive effects. TNF antagonists, for example, are associated with an increased risk of infection, especially tuberculosis reactivation.
There is one positive “new think” in conventional treatment, though, which is the idea that gentle exercise can help arthritis symptoms. Many arthritis clinics now offer water therapy. Patients undergo gentle stretching and exercise in a swimming pool, which helps take the weight off painful knee and hip joints. It’s been shown that gentle exercise such as swimming and walking can help maintain flexibility in joints so that patients require less care.
In contrast to the conventional drug treatments, a holistic approach to either kind of arthritis is to identify the causative factors and detoxify the body as a means of controlling and reversing the disease. Natural products and non-drug therapies are used whenever possible to avoid the toxicity of “designer drugs.” I remember a patient in her sixties who came in absolutely racked with osteoarthritis, leaning on a cane and positively creaking when she slowly settled into a chair in my office. She had diffuse osteoarthritis in the shoulders, the knees and the feet that seemed fairly well advanced. I was concerned that she might have so much destruction of joint tissue that even if we could reduce the inflammation she’d still be left with creaky, deformed joints. We treated her with diet changes, acupuncture and specific oral nutrients, and she had an incredible turnaround within six months. At this point she needs only occasional maintenance acupuncture treatments, once every month. By no means do all patients respond as magnificently as she did, but I usually have an even more optimistic prognosis for patients who have only mild or localized arthritis. Let’s take a closer look at some alternative treatments.
Diet modification
Monolithic groups such as the Arthritis Foundation long held the position that dietary cures for arthritis were quackery. But they have recently been forced to soften their position in light of scientific evidence that dietary approaches do make a difference. Dietary “cures” for RA, and even osteoarthritis, have long been touted by folk medicine. Researchers began to compile scientific confirmation as early as 1911, with studies showing that restricted diet programs could produce remission of arthritis. The subject is a difficult one because different patients respond in different ways to various dietary manipulations. In truth, arthritis can be considered the final common end point of a variety of factors. This may explain why not all patients respond to dietary intervention alone.
Patients who are obese must make permanent dietary changes. Experimental trials have shown that if arthritis patients go on a hypoallergenic diet in which common food allergens are eliminated and substituted by a neutral synthetic food supplement such as Vivonex, their symptom scores improve markedly. Some studies have demonstrated the value of specific allergy testing of the skin or the blood to predict which food should be eliminated. Other studies have underscored the value of a low-fat diet based largely on fresh fruits, vegetables, cereal grains and legumes. Some trials have produced benefits when patients eliminate cereal grains altogether and emphasize proteins rich in polyunsaturated fat, such as fish and nuts. These low-carbohydrate diets may help because they suppress growth of harmful or immune-active intestinal bacteria.
One diet that works with some people is to eliminate the nightshade foods, which include tomatoes, potatoes, eggplant, peppers, paprika and cayenne. Tobacco also is a nightshade. In fact, there’s an animal model for arthritis: If cows are mistakenly given fodder that is heavily laced with wild-growing nightshade family plants, they actually develop a type of osteoarthritis. Anyone who suffers from arthritis could try avoiding these foods for a couple of months and then gradually reintroduce them to see whether they provoke symptoms.
Fasting has been shown to be therapeutic in some cases for both osteoarthritis and RA. Fasting allows the body to detoxify and offers a break from the onslaught of food antigens that may trigger joint inflammation. This traditional therapy seems to work in many cases—you go on a fast and your arthritis gets better. It may help because of food intolerances, or it may allow your gut to stop supporting the growth of certain harmful bacteria or fungi that produce toxic byproducts that somehow trigger the arthritis. In the “leaky gut syndrome,” a stressed intestinal tract may become permeable to microscopic food protein particles, allowing them to enter the bloodstream and set up an immune reaction in the tissue. An overgrowth of harmful intestinal bacteria or yeast, otherwise known as dysbiosis, may compound the problem. Detoxification regimens sometimes use fibers such as psyllium or absorbent clays such as bentonite, with or without the assistance of colonic irrigations or enemas. It also may help to replace harmful intestinal flora with cultures of benign bacteria such as Lactobacillus acidophilus from yogurt or other probiotic supplements.
Dietary supplements
Several nutrients affect arthritic symptoms, some by reducing inflammation and others by retarding the degeneration of cartilage or normalizing immune reactions. Some of these supplements include MSM, InflamaSYN, glucosamine, chondroitin, ASU, Lyprinol, SAM-e, Undenatured Collagen Type II and EGCG. In fact, recent results of a clinical trial sponsored by the National Institutes of Health (NIH) showed that the combined use of glucosamine and chondroitin provided significant relief from osteoarthritis pain. This study, called the Glucosamine/Chondroitin Arthritis Intervention Trial (GAIT) adds to the vast majority of more than 50 published clinical trials that demonstrate the benefits and safety of these two supplements. Moreover, preliminary results from another trial in Europe called the glucosamine Unum in Die Efficacy Trial (GUIDE) found that glucosamine was more effective than acetaminophen (Tylenol) in relieving osteoarthritis pain. I think these studies offer a stunning vindication of the natural approach to arthritis, at the very time that conventional therapies such as Vioxx and Bextra have fallen by the wayside.
The omega-3 oils, present in flaxseed oil and in cold-water fish such as salmon, herring, trout, mackerel, sardines and cod liver, are especially helpful in relieving morning stiffness and tender joints. GLA (gamma-linolenic acid), an omega-6 oil that is present in primrose oil, borage oil and black currant seed oil, has been shown to augment the anti-inflammatory effect of the omega-3 oils.
Herbal remedies
Many Western herbs are beneficial in the treatment of arthritis. It’s worth remembering that the discovery of aspirin was predicated on the traditional folk wisdom that the bark of the white willow could reduce aches and pains. White willow bark is high in salicylic acid, the active ingredient of aspirin. Herbs that can play an important role in treating arthritis include curcumin (extracted from the spice turmeric), ashwagandha, Boswellin, Jamaican dogwood, devil’s claw, licorice, ginger and yucca. Many are available in easy-to-use alcohol or glycerine tinctures or in an encapsulated freeze-dried form. Capsaicin, an extract of cayenne pepper, is a topical counterirritant cream that provides relief from joint pain. It’s an alternative to the traditional menthol-containing ointments and may be slightly more effective for some.
Forward-thinking complementary medical practices utilize intravenous drip therapies to treat arthritis, among other conditions. At the Hoffman Center, our “Joint Protocol I.V.” which includes important vitamins and minerals such as vitamin C, copper, magnesium, manganese and selenium, to name a few, has proved effective in alleviating the debilitating symptoms of osteoarthritis and RA in many of our patients.
A look to the future
It may take some time, but I expect that eventually even the medical establishment will grant that using natural substances—such as vitamins and nutrients, herbs, and antigen feeding—may be beneficial in treating and preventing musculoskeletal ailments.
At present, arthritis remains a big unknown. We are still not clear about exactly what causes it, and we may not yet be looking in the right places. For now, if you want a quick fix, you can take the NSAIDs and other drugs but at the risk of actually worsening the underlying physiology of joint degeneration. Natural therapies such as antioxidants, the omega-3 and omega-6 oils, and the others I’ve mentioned don’t provide instantaneous pain relief, but they do gradually alter the underlying physiology of inflammation and are safer in the long run. Again, this highlights the fundamental divergence between the conventional medical approach and the holistic approach. Since alternative therapies don’t ameliorate pain so quickly, you have to tough it out for a while, but the results are ultimately more gratifying.
Though doctors and patients alike show a lot of enthusiasm for high-tech surgeries and imaging techniques, there are some good low-tech therapies that are probably being underutilized. Methods such as the Alexander technique can be very helpful for developing a heightened body awareness and for overcoming habits of body posture that may create physical stress and even chronic pain. Chiropractors could do more useful preventive work against the degenerative processes of aging that work on the spine and which may not only affect spinal health but the flow of neurological energy throughout the body.
We are undergoing a sea change in our attitudes toward both osteoarthritis and rheumatoid arthritis in admitting that there may be a nutritional component, an allergic component and an infectious component to the disease, and in recognizing that the use of natural substances such as vitamins, nutrients and antigen feeding can be used to treat it. Probably the future breakthrough in the treatment of arthritis will be an immune modulating therapy that will break the inflammatory cascade at the source, at the cellular level and bring the immune response back into balance.
1. Centers for Disease Control and Prevention [On-line]. The Burden of Arthritis, United States. Available at: www.cdc.gov/nccdphp/burdenbook2004/Section05/arthritis.htm. Accessed December 3, 2005.
2. Holick MF. The vitamin D epidemic and its health consequences. J Nutr. 2005;135(11):2739S-48S.
3. Mikuls TR, Cerhan JR, Criswell LA, et al. Coffee, tea, and caffeine consumption and risk of rheumatoid arthritis: Results from the Iowa Womenýs Health Study. Arthritis Rheum. 2002;46:83-91.
4. Arthritis Foundation [On-line]. Reiter’s Syndrome (Reactive Arthritis). Available at: www.arthritis.org/conditions/DiseaseCenter/reiters.asp. Accessed December 6, 2005.
5. Huang, HY, Appel LJ, Choi MJ, et al. The effects of vitamin C supplementation on serum concentrations of uric acid: Results of a randomized controlled trial. Arthritis Rheum. 2005;52(6):1843-7.
6. American Family Physician [On-line]. Diagnosis and Management of Rheumatoid Arthritis. Available at: www.aafp.org/afp. Accessed December 3, 2005.
7. Arthritis Foundation [On-line]. Drug News: In a Class by Itself. Available at: www.arthritis.org/resources/arthritistoday/2005_archives/2005. Accessed December 6, 2005.
Though we think of declining estrogen as the hallmark of menopause, it's actually common for…

Up to 12 percent of Americans have ulcers at some point in life. Peptic ulcers…
Gallbladder disease is a modern illness. An estimated 20 million Americans have gallbladder disease. The…

Lately, I’ve been sharing with Intelligent Medicine listeners that I’ve been augmenting my diet with…
Q: I am a 77-year-old woman. On recent bone density test, lumbar spine results range…

The 1973 sci-fi movie Soylent Green depicts a dystopian future in which over-population and environmental…

Q&A with Leyla, Part 1: Copper Supplements

Our virtual voicemail is open 24/7, so there's no need to wait to submit your questions for Dr. Hoffman. Leave a message, and you may hear your question featured on the Intelligent Medicine radio program!